International Neuromodulation Society Webinars
The International Neuromodulation Society is pleased to offer webinars for members featuring renowned experts reviewing the latest research, therapies and best practices and offering guidance on patient safety, patient selection and device selection to optimize treatment outcomes and reduce adverse events – all of which are of paramount importance in the field of neuromodulation.
Learn more about participation, recordings, and CME credit.
Future webinar topics and dates:
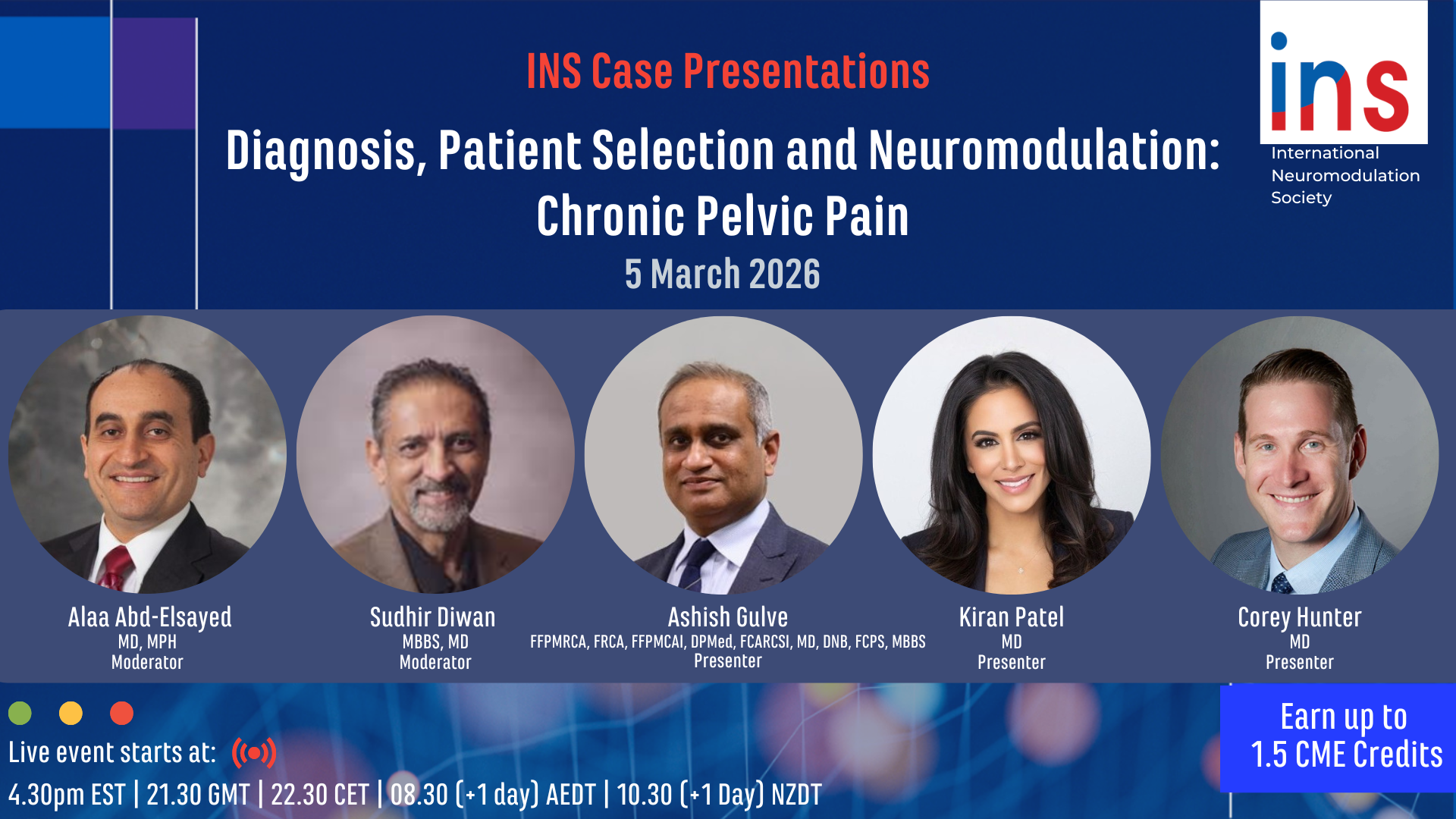
Thurs. March 5, 2026
4:30pm EDT/21:30 BST/22:30 CEST/06:30 (+1 day) AEST/08:30 (+1 day) NZST
Moderators: Sudir Diwan, MB,BS, MS and Alaa Abd-Elsayed, MD, MPH
Topics and Faculty:
1.) Diagnosis of Chronic Pelvic Pain - Ashish Gulve, FFPMRCA, FRCA, FFPMCAI, DPMed, FCARCSI, MD, DNB, FCPS, MBBS
2.) Chronic Pelvic Pain Patient Selection for Neuromodulation - Kiran Patel , MD
3.) Procedure – CPP Specific Issues - Corey Hunter, MD
CME Credit
This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through a collaboration between Elsevier, Inc. and the International Neuromodulation Society.
The Elsevier Office of CME is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
The Elsevier Office of CME designates this educational material for a maximum of 1.5 AMA PRA Category 1 Credit(s)™. Physicians should only claim credit commensurate with the extent of their participation in the activity.
This webinar will be recorded. If you have missed the previous INS webinars, you can watch the videos on demand on the INS members' website. Each recorded presentation is eligible for CME credits for up to sixty (60) days after the date of a webinar event.

Continuing Medical Education Content Reviewer
Stana Bojanic, BSc (Hons), MB BS, FRCS (SN)
Past President, Neuromodulation Society of the UK and Ireland
Consultant Neurosurgeon and Spinal Surgeon, Oxford University Hospitals Trust and the Manor Hospital
Past Webinars
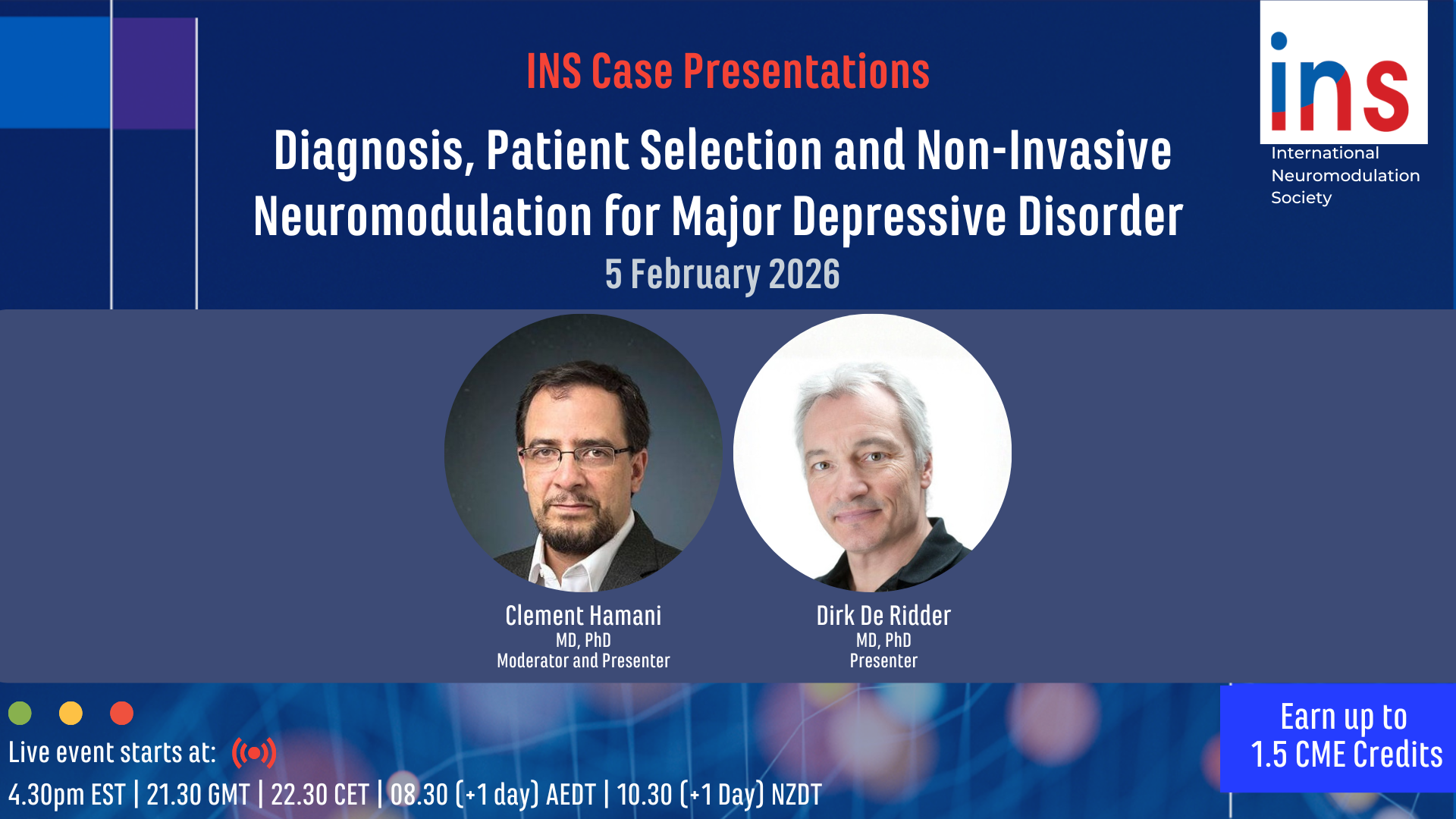
Case Presentations: Diagnosis, Patient Selection and Non-Invasive Neuromodulation for Major Depressive Disorder
Thurs. February 5, 2026
Moderators: Clement Hamani, MD, PhD and Christopher Austelle, MD
Topics and Faculty:
1.) Diagnosis of MDD - Clement Hamani, MD, PhD
2.) MDD Patient Selection for Neuromodulation - Dirk De Ridder, MD, PhD
3.) Procedure – Christopher Austelle, MD
Case Presentations: Diagnosis, Patient Selection and Neuromodulation: Refractory Headache
Thurs. January 8, 2026
Moderators: Salim Hayek, MD, PhD and Ryan S. D'Souza MD
Topics and Faculty:
1.) Diagnosis of Refractory Headache - Peter Goadsby, MBBS, MD, PhD, DSc, FRACP, FRCP, FMedSci, FRS
2.) Refractory Headache Patient Selection for Neuromodulation - Christopher Gilligan, MD, MBA
3.) Procedure – Refractory Headache Specific Issues - Konstantin Slavin, MD
Case Presentations: Diagnosis, Patient Selection and Neuromodulation for Refractory Angina
Thurs. Dec 4, 2025
Moderators: Siamak Salavatian MEng, PhD
Topics and Faculty:
1.) Diagnosis of Refractory Angina - Hans A. van Suijlekom, MD, PhD
2.) RA Patient Selection for Neuromodulation - Kliment Gatzinsky, MD, PhD
3.) Procedure – RA Specific Issues - Georgios K. Matis MD, MSc, PhD
Case Presentations: Diagnosis, Patient Selection and Neuromodulation for Postherpetic Neuralgia
Thurs. Nov. 6, 2025
Moderators: Eellan Sivanesan, MD, FASA and Salim Hayek, MD, PhD
Topics and Faculty:
1.) Diagnosis of PHN - Kiran Patel, MD
2.) PHN Patient Selection for Neuromodulation - Prasad Shirvalkar, MD, PhD
3.) Procedure – PHN Specific Issues - Ryan S. D'Souza MD
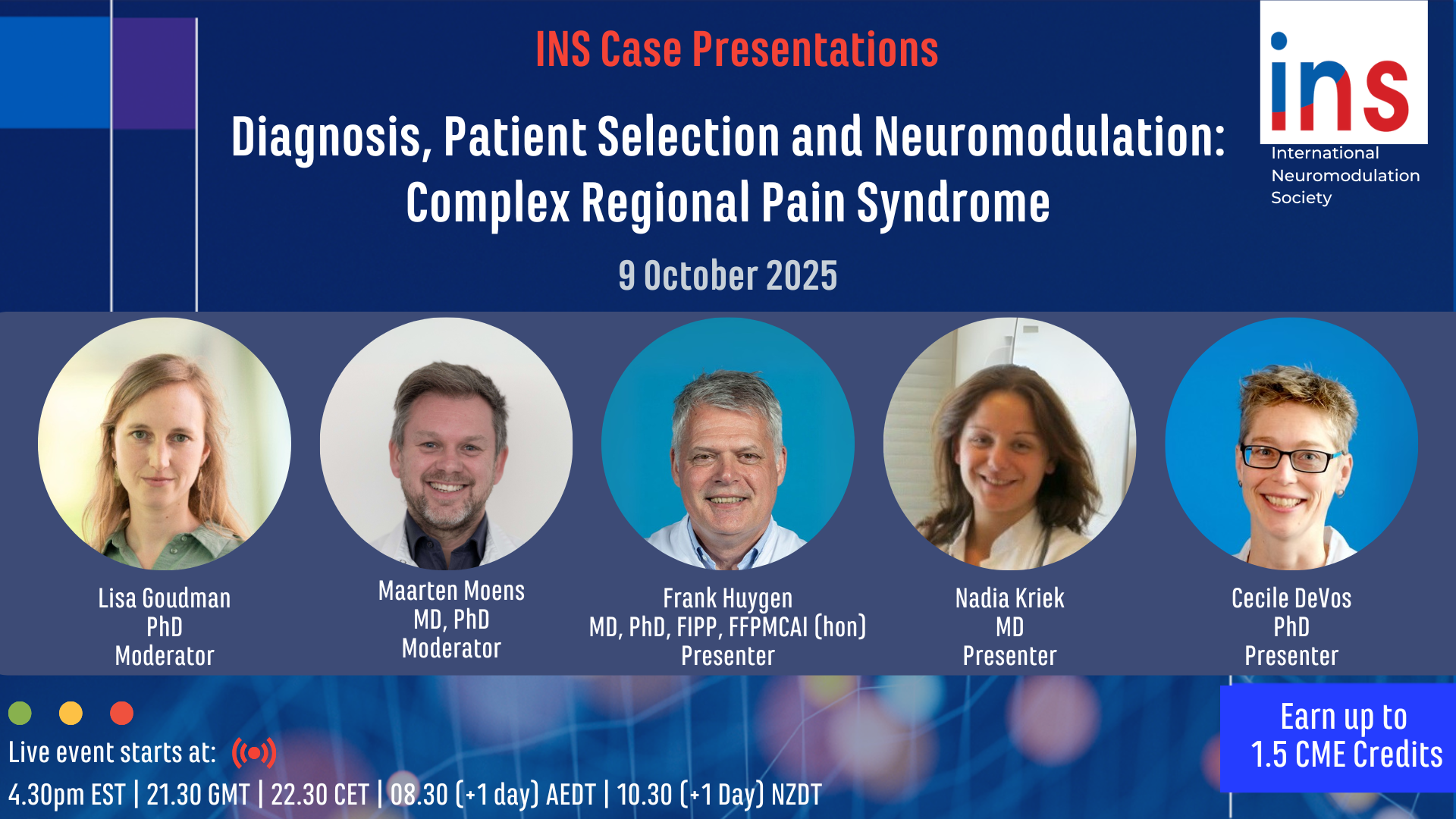
Case Presentations: Diagnosis, Patient Selection and Neuromodulation for Complex Regional Pain Syndrome
Thurs. Oct. 9, 2025
Moderators: Maarten Moens, MD, PhD and Lisa Goudman, PhD
Topics and Faculty:
1.) Diagnosis of CRPS - Frank Huygen, MD, PhD, FIPP, FFPMCAI (hon)
2.) CRPS Patient Selection for Neuromodulation - Nadia Kriek, MD
3.) Procedure – CRPS Specific Issues - Cecile DeVos, PhD
INS Virtual Debate: Ethical Issues in Neuromodulation for Cognitive Function
Thurs. Sept. 4, 2025
Moderators: Robert Levy, MD, PhD and James FitzGerald, MA, BM BCh, FRCS(SN), PhD
Topics and Faculty:
1.) Neuromodulation Ethical Issues should not Impact the Progress of Neuromodulation Research and Therapy: Pursuing Supra-Normal Outcomes - Laura Cabrera, PhD
2.) Neuromodulation Therapies should be Limited to Restoring Normal Function - Veljko Dubljevic, PhD
3.) Neuromodulation Therapies should not be Offered to Subjects with Limited Cognition - TBC
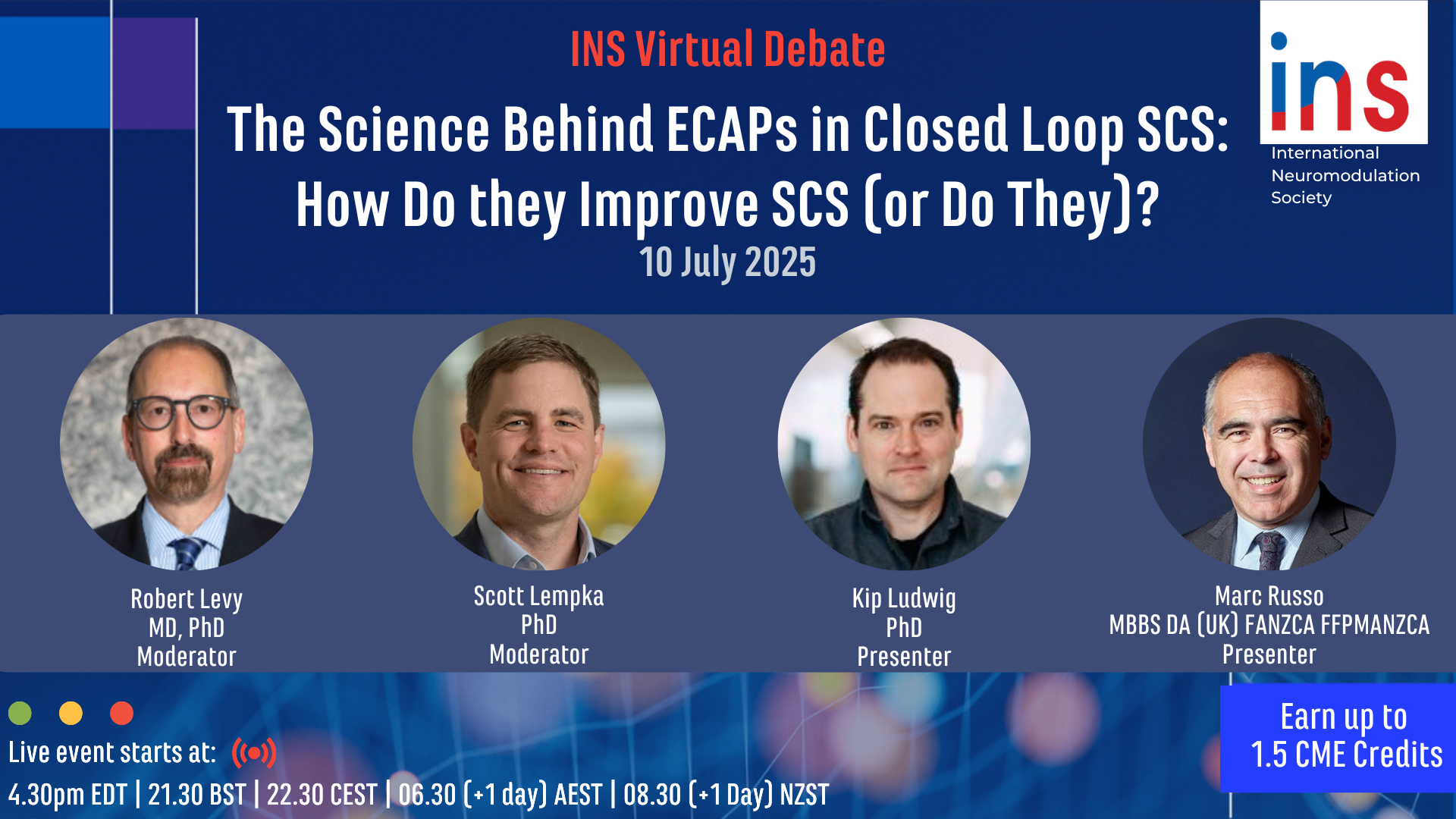
INS Virtual Debate: The Science Behind ECAPs in Closed Loop SCS: How Do they Improve SCS (or Do They)?
Thurs. July 10, 2025
Moderators: Robert Levy, MD, PhD and Scott Lempka, PhD
Panelist: James FitzGerald, MA BM BCh FRCS(SN) PhDTopics and Faculty:
1.) Limitations to the Current Use of ECAPs for SCS - Kip Ludwig, PhD
3.) ECAPs Science and their Value in SCS - Marc Russo, MBBS DA (UK) FANZCA FFPMANZCA
INS Debate - What is the Best Neuromodulation Therapy for Depression?
Thurs. June 5, 2025

Moderators: Nir Lipsman, MD, PhD, FRCSC and Clement Hamani, MD
Topics and Faculty:
1.) Transcranial Magnetic Stimulation - Peter Giacobbe, MD, MSc, FRCPC
2.) Vagus Nerve Stimulation - Scott T. Aaronson, MD
3.) Deep Brain Stimulation - Sameer Anil Sheth, MD, PhD
INS Debate – What is the Best Neuromodulation Treatment for Drug Resistant Epilepsy?
Thurs. May 8, 2025

Moderators: Kristl Vonck, MD, PhD, FEAN and Arthur Cukiert, MD, PhD
Topics and Faculty:
1) Vagus Nerve Stimulation - George M. Ibrahim, MD, PhD, FRCSC, FAANS, FACS
2) Deep Brain Stimulation - Robert Fisher, MD, PhD
3) Responsive Neurostimulation - Robert E. Gross, MD, PhD
INS Debate – What is the Best Neuromodulation Treatment for Chronic Migraine and Cluster Headache?
Thurs. April 3, 2025
Moderators: Christopher J. Gilligan MD, MBA and Konstantin Slavin, MD
Topics and Faculty:
1) Occipital Nerve Stimulation - Erkan Kurt, MD
2) Combined Occipital and Trigeminal - Samer Narouze, MD, PhD
3) Sphenopalatine Ganglion Stimulation - Konstantin Slavin, MD
INS Debate: What is the Best Neuromodulation Treatment for Post Surgical Pain Syndrome?
Thurs. March 6, 2025
Moderators: David Provenzano, MD and Jonathan Hagedorn, MD
Topics and Faculty
1) Pulsed Radiofrequency for Post Surgical Pain Syndrome - Laurens Peene, MD, FIPP
2) Spinal Cord Stimulation for Post Surgical Pain Syndrome - Ryan D’Souza, MD
3) Dorsal Root Ganglion Stimulation for Post Surgical Pain Syndrome - Kiran Patel, MD
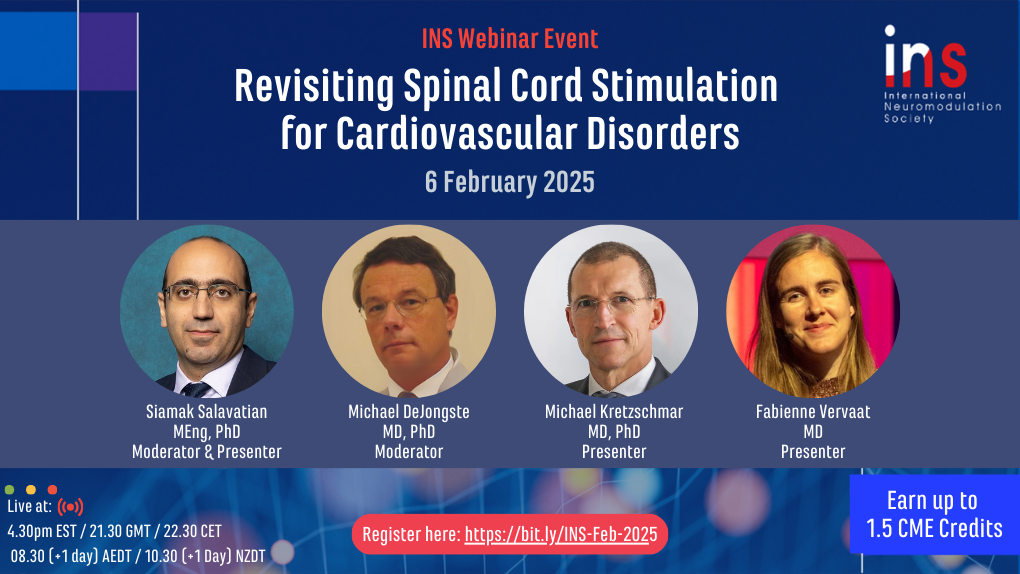
Revisiting Spinal Cord Stimulation for Cardiovascular Disorders
Thurs. Feb 6, 2025
Moderators: Siamak Salavatian, MEng, PhD and Michael DeJongste, MD, PhD Topics and Faculty: 1) Comparing the Memory Effects of Low and High-Frequency Thoracic Spinal Cord Stimulation on Spinal Neural Network in a Myocardial Infarction Porcine Model - Siamak Salavatian, MEng, PhD 2) Spinal Neuromodulation for Peripheral Arterial Disease of Lower Extremities: A Ten-Year Retrospective Analysis - Michael Kretzschmar, MD, PhD 3) Single-Center Experience With High-Density Spinal Cord Stimulation in Patients With Refractory Angina Pectoris - Fabienne Vervaat, MD
Background Articles:
Salavatian S, Wong B, Kuwabara Y, Fritz JR, Varghese CG, Howard-Quijano K, Armour JA, Foreman RD, Ardell JL, Mahajan A. Comparing the Memory Effects of 50-Hz Low-Frequency and 10-kHz High-Frequency Thoracic Spinal Cord Stimulation on Spinal Neural Network in a Myocardial Infarction Porcine Model. Neuromodulation. 2024 Oct;27(7):1177-1186. doi: 10.1016/j.neurom.2024.06.002. Epub 2024 Jul 31. PMID: 39078348.
Kretzschmar M, Okaro U, Schwarz M, Reining M, Lesser T. Spinal Neuromodulation for Peripheral Arterial Disease of Lower Extremities: A Ten-Year Retrospective Analysis. Neuromodulation. 2024 Oct;27(7):1240-1250. doi: 10.1016/j.neurom.2023.10.186. Epub 2024 Jan 1. PMID: 38165292.
Vervaat FE, van Suijlekom H, Wijnbergen IF. Single-Center Experience With High-Density Spinal Cord Stimulation in Patients With Refractory Angina Pectoris. Neuromodulation. 2024 Oct;27(7):1234-1239. doi: 10.1016/j.neurom.2022.11.006. Epub 2022 Dec 10. PMID: 36513588.
State of the Art: Neuromodulation for Major Depression
Thurs. Jan. 9, 2025
4:30pm EST/21:30 GMT/22:30 CET/08:30 (+1 day) AEDT/10:30 (+1 day) NZDT
Moderators: Helen Mayberg, MD and James FitzGerald, PhD Topics and Faculty: 1) Novel TMS Protocols for Depression - Noah S. Philip MD, DFAPA 2) VNS for Depression: RECOVER Study - Charles Conway, MD 3) Closed Loop DBS in Depression - Kristin Sellers, PhD
Background Articles:
van Rooij SJH, Arulpragasam AR, McDonald WM, Philip NS. Accelerated TMS - moving quickly into the future of depression treatment. Neuropsychopharmacology. 2023 May 22. doi: 10.1038/s41386-023-01599-z. Epub ahead of print. Erratum in: Neuropsychopharmacology. 2023 Aug 28;: PMID: 37217771.
Conway CR, Aaronson ST, Sackeim HA, Tran Q, Yates L, Rush AJ, et al. Vagus nerve stimulation in treatment-resistant depression: A one-year, randomized, sham-controlled trial. Brain Stimulation. Dec. 18, 2024. DOI: 10.1016/j.brs.2024.12.1191.
Scangos KW, Khambhati AN, Daly PM, Makhoul GS, Sugrue LP, Zamanian H, Liu TX, Rao VR, Sellers KK, Dawes HE, Starr PA, Krystal AD, Chang EF. Closed-loop neuromodulation in an individual with treatment-resistant depression. Nat Med. 2021 Oct;27(10):1696-1700. doi: 10.1038/s41591-021-01480-w. Epub
The Polyanalgesic Consensus Conference (PACC)®: Updates on Clinical Pharmacology and Comorbidity Management with Intrathecal Drug Delivery for Cancer Pain
Thurs. Dec. 5, 2024
4:30pm EST/21:30 GMT/22:30 CET/08:30 (+1 day) AEDT/10:30 (+1 day) NZDT
Moderators: Lawrence Poree, MD, PhD, MPH and Salim Hayek, MD, PhD Topics and Faculty:
1) Psychological Assessment and Support for the Cancer Patient Considering IT Therapy – Jill Osborn, BSc (PT), PhD, MD, FRCPC (Anesthesiology)
2) Update: Management of Comorbid Conditions with IT Therapy in the Cancer Patient – John Hagedorn, MD
3) Update: Review of IT Medications for the Treatment of Cancer Patient – Jay Grider, DO, PhD, MBA
4) Disease Related Assessment for IT Therapy – Peter Staats, MD, MBA
5) Update: Trialing and Maintenance of IT Therapy in the Cancer Patient – Salim Hayek, MD, PhD
Background Article:
Deer TR, Hayek SM, Grider JS, Pope JE, Brogan SE, Gulati A, Hagedorn JM, Strand N, Hah J, Yaksh TL, Staats PS, Perruchoud C, Knezevic NN, Wallace MS, Pilitsis JG, Lamer TJ, Buchser E, Varshney V, Osborn J, Goel V, Simpson BA, Lopez JA, Dupoiron D, Saulino MF, McDowell GC 2nd, Piedimonte F, Levy RM. The Polyanalgesic Consensus Conference (PACC)®: Updates on Clinical Pharmacology and Comorbidity Management in Intrathecal Drug Delivery for Cancer Pain. Neuromodulation. 2024 Sep 20:S1094-7159(24)00670-6. doi: 10.1016/j.neurom.2024.08.006. Epub ahead of print. PMID: 39297833.
The Polyanalgesic Consensus Conference (PACC)®: Intrathecal Drug Delivery Guidance on Safety and Therapy Optimization
Thurs. Nov. 7, 2024
Moderators: Lawrence Poree, MD, PhD, MPH and PD. Dr. med Christophe Perruchoud Topics and Faculty:
1) Updates on Trialing and Implant Procedures - Salim Hayek, MD, PhD
2) Updates on Perioperative and Postoperative Patient Management - Jay Grider, DO, PhD, MBA
3) Updates on Intrathecal Pharmacotherapy - John Hagedorn, MD
4) Updates on Drug Delivery System Issues - Lawrence Poree, MD, PhD, MPH
5) Updates on Health Care Economic Issues – Julie Pilitsis, MD, PhD, MBA
Background Article:
Deer TR, Hayek SM, Grider JS, Hagedorn JM, McDowell GC 2nd, Kim P, Dupoiron D, Goel V, Duarte R, Pilitsis JG, Leong MS, De Andrés J, Perruchoud C, Sukumaran H, Abd-Elsayed A, Saulino M, Patin D, Poree LR, Strand N, Gritsenko K, Osborn JA, Dones I, Bux A, Shah JM, Lindsey BL, Shaw E, Yaksh TL, Levy RM. The Polyanalgesic Consensus Conference (PACC)®: Intrathecal Drug Delivery Guidance on Safety and Therapy Optimization When Treating Chronic Noncancer Pain. Neuromodulation. 2024 May 13:S1094-7159(24)00066-7. doi: 10.1016/j.neurom.2024.03.003. Epub ahead of print. PMID: 38752946.
The Neurostimulation Appropriateness Consensus Committee (NACC) ®: Recommendations for Spinal Cord Stimulation Long-Term Outcome Optimization and Salvage Therapy
Thurs. Oct. 10, 2024
Moderators:Robert Levy, MD, PhD and Konstantin Slavin, MD Topics and Faculty:
1) Spinal Cord Stimulation Habituation and Tolerance - Salim Hayek, MD, PhD 2) Patient Evaluation Procedures in the Setting of Loss of Efficacy of SCS - Jon Hagedorn, MD 3) Spinal Cord Stimulation Therapy Optimization Strategies with Existing Systems - Christopher Gilligan, MD, MBA 4) Spinal Cord Stimulation Therapy Optimization with Device Replacement and Upgrade - Tim Lamer, MD
Background Articles:
Dr Timothy Ray Deer. Marc Russo, FFPMANZCA; Jay S. Grider, DO, PhD; Dawood Sayed, MD; Tim J. Lamer, MD; David Dickerson, MD; Jonathan M. Hagedorn, MD; Petersen A. Erika, MD; Michael A. Fishman, MD, PhD; James FitzGerald, FRCS, PhD; Ganesan Baranidharan, MBBS; Dirk De Ridder, MD, PhD; Krishnan V. Chakravarthy, MD, PhD; Adnan Al-Kaisy, MB, ChB; Corey W. Hunter, MD; Eric Buchser, MD; Kenneth Chapman, MD; Chris Gilligan, MD, MBA; Salim M. Hayek, MD, PhD; Simon Thomson, MBBS; Natalie Strand, MD; Jessica Jameson, MD; Thomas T. Simopoulos, MD, MA; Ajax Yang, MD; Olivier De Coster, MD, FIPP; Fabian Cremaschi, Prof. Dr.; Paul J. Christo, MD, MBA; Vishal Varshney, MD; Stana Bojanic, MB, BS, FRCS; Robert M. Levy, MD, PhD. The Neurostimulation Appropriateness Consensus Committee (NACC)®: Recommendations for Spinal Cord Stimulation Long-Term Outcome Optimization and Salvage Therapy. Neuromodulation. 2024 June 19. https://doi.org/10.1016/j.neurom.2024.04.006
Deer TR, Russo MA, Grider JS, Pope J, Rigoard P, Hagedorn JM, Naidu R, Patterson DG, Wilson D, Lubenow TR, Buvanendran A, Sheth SJ, Abdallah R, Knezevic NN, Schu S, Nijhuis H, Mehta P, Vallejo R, Shah JM, Harned ME, Jassal N, Gonzalez JM, Pittelkow TP, Patel S, Bojanic S, Chapman K, Strand N, Green AL, Pahapill P, Dario A, Piedimonte F, Levy RM. The Neurostimulation Appropriateness Consensus Committee (NACC): Recommendations for Surgical Technique for Spinal Cord Stimulation. Neuromodulation. 2022 Jan;25(1):1-34. doi: 10.1016/j.neurom.2021.10.015. PMID: 35041578.
Deer TR, Russo MA, Sayed D, Pope JE, Grider JS, Hagedorn JM, Falowski SM, Al-Kaisy A, Slavin KV, Li S, Poree LR, Eldabe S, Meier K, Lamer TJ, Pilitsis JG, De Andrés J, Perruchoud C, Carayannopoulos AG, Moeschler SM, Hadanny A, Lee E, Varshney VP, Desai MJ, Pahapill P, Osborn J, Bojanic S, Antony A, Piedimonte F, Hayek SM, Levy RM. The Neurostimulation Appropriateness Consensus Committee (NACC)®: Recommendations for the Mitigation of Complications of Neurostimulation. Neuromodulation. 2024 Jun 13:S1094-7159(24)00075-8. doi: 10.1016/j.neurom.2024.04.004. Epub ahead of print. PMID: 38878054.
The Neurostimulation Appropriateness Consensus Committee (NACC) ®:
Recommendations for the Mitigation of Complications of Neurostimulation
Thurs. Sept. 5, 2024
4:30pm EST/21:30 GMT/22:30 CET/08:30 (+1 day) AEDT/10:30 (+1 day) NZDT
Moderators:Jay Grider, MD, PhD, MBA and Tim Lamer, MD Topics and Faculty:
1) Evidence Ranking and Recommendation Development - Timothy Deer, MD 2) Update: Evidence Based Approach to Hemorrhagic Complications of Neurostimulation Procedures - Tim Lamer, MD 3) Update: Evidence Based Approach to Infectious Complications of Neurostimulation Procedures - Salim Hayek, MD, PhD 4) Update: Evidence Based Approach to Neurologic Injury Following Neurostimulation Procedures - Jonathan M. Hagedorn, MD 5) Update: New Issues Raised in the 2024 NACC - Jay Grider, DO, PhD, MBA
Background Articles:
Deer TR, Russo M, Grider JS, Pope J, Hagedorn JM, Weisbein J, Abd-Elsayed A, Benyamin R, Raso LJ, Patel KV, Provenzano D, Kim PS, Amirdelfan K, Bolash R, Steegers M, Sullivan R, Verrills P, Carlson J, Kapural L, Diwan S, Barolat G, Pahapill PA, De Andres J, Raslan AM, Lopez JA, Leong MS, Attias MB, Teddy P, Green AL, Dario A, Piedimonte F, Chapman KB, Tomycz ND, FitzGerald J, Gatzinsky K, Varshney V, Gish B, Lindsey BL, Buvanendran A, Lamer TJ, Slavin KV, Levy RM. The Neurostimulation Appropriateness Consensus Committee (NACC): Recommendations on Best Practices for Cervical Neurostimulation. Neuromodulation. 2022 Jan;25(1):35-52. doi: 10.1016/j.neurom.2021.10.013. Erratum in: Neuromodulation. 2022 Apr;25(3):482. doi: 10.1016/j.neurom.2022.01.001. PMID: 35041587.
Deer TR, Russo MA, Grider JS, Pope J, Rigoard P, Hagedorn JM, Naidu R, Patterson DG, Wilson D, Lubenow TR, Buvanendran A, Sheth SJ, Abdallah R, Knezevic NN, Schu S, Nijhuis H, Mehta P, Vallejo R, Shah JM, Harned ME, Jassal N, Gonzalez JM, Pittelkow TP, Patel S, Bojanic S, Chapman K, Strand N, Green AL, Pahapill P, Dario A, Piedimonte F, Levy RM. The Neurostimulation Appropriateness Consensus Committee (NACC): Recommendations for Surgical Technique for Spinal Cord Stimulation. Neuromodulation. 2022 Jan;25(1):1-34. doi: 10.1016/j.neurom.2021.10.015. PMID: 35041578.
Deer TR, Russo MA, Sayed D, Pope JE, Grider JS, Hagedorn JM, Falowski SM, Al-Kaisy A, Slavin KV, Li S, Poree LR, Eldabe S, Meier K, Lamer TJ, Pilitsis JG, De Andrés J, Perruchoud C, Carayannopoulos AG, Moeschler SM, Hadanny A, Lee E, Varshney VP, Desai MJ, Pahapill P, Osborn J, Bojanic S, Antony A, Piedimonte F, Hayek SM, Levy RM. The Neurostimulation Appropriateness Consensus Committee (NACC)®: Recommendations for the Mitigation of Complications of Neurostimulation. Neuromodulation. 2024 Jun 13:S1094-7159(24)00075-8. doi: 10.1016/j.neurom.2024.04.004. Epub ahead of print. PMID: 38878054.
Dr Timothy Ray Deer. Marc Russo, FFPMANZCA; Jay S. Grider, DO, PhD; Dawood Sayed, MD; Tim J. Lamer, MD; David Dickerson, MD; Jonathan M. Hagedorn, MD; Petersen A. Erika, MD; Michael A. Fishman, MD, PhD; James FitzGerald, FRCS, PhD; Ganesan Baranidharan, MBBS; Dirk De Ridder, MD, PhD; Krishnan V. Chakravarthy, MD, PhD; Adnan Al-Kaisy, MB, ChB; Corey W. Hunter, MD; Eric Buchser, MD; Kenneth Chapman, MD; Chris Gilligan, MD, MBA; Salim M. Hayek, MD, PhD; Simon Thomson, MBBS; Natalie Strand, MD; Jessica Jameson, MD; Thomas T. Simopoulos, MD, MA; Ajax Yang, MD; Olivier De Coster, MD, FIPP; Fabian Cremaschi, Prof. Dr.; Paul J. Christo, MD, MBA; Vishal Varshney, MD; Stana Bojanic, MB, BS, FRCS; Robert M. Levy, MD, PhD. The Neurostimulation Appropriateness Consensus Committee (NACC)®: Recommendations for Spinal Cord Stimulation Long-Term Outcome Optimization and Salvage Therapy. Neuromodulation. 2024 June 19. https://doi.org/10.1016/j.neurom.2024.04.006
This webinar has been supported by a grant from Nevro.
State of the Art: Neuromodulation for Obsessive Compulsive Disorder
Thurs., July 11, 2024
4:30pm EST/21:30 GMT/22:30 CET/08:30 (+1 day) AEDT/10:30 (+1 day) NZDT
Moderators:
Veerle Visser-Vandewalle, MD, PhD and Kendall Lee, MD, PhD
Topics and Faculty:
1) Effects of deep brain stimulation on brain function in obsessive-compulsive disorder: From Animal Models to Patients - Damiaan Denys, PhD
2) Efficacy of deep brain stimulation for treatment-resistant OCD: Systemic Review and Metaanalys - Garrett Paul Banks, MD
3) Brain Structures and Networks Underlying Treatment Response to Deep Brain Stimulation Targeting the Inferior Thalamic Peduncle in Obsessive-Compulsive Disorder - Jürgen Germann, PhD
Background Articles:
Bangel KA, Bais M, Eijsker N, Schuurman PR, van den Munckhof P, Figee M, Smit DJA, Denys D. Acute effects of deep brain stimulation on brain function in obsessive-compulsive disorder. Clin Neurophysiol. 2023 Apr;148:109-117. doi: 10.1016/j.clinph.2022.12.012. Epub 2023 Jan 23. PMID: 36774324.
Gadot R, Najera R, Hirani S, Anand A, Storch E, Goodman WK, Shofty B, Sheth SA. Efficacy of deep brain stimulation for treatment-resistant obsessive-compulsive disorder: systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2022 Sep 20:jnnp-2021-328738. doi: 10.1136/jnnp-2021-328738. Epub ahead of print. Erratum in: J Neurol Neurosurg Psychiatry. 2023 Oct;94(10):e1. PMID: 36127157.
Germann J, Boutet A, Elias GJB, Gouveia FV, Loh A, Giacobbe P, Bhat V, Kucharczyk W, Lozano AM. Brain Structures and Networks Underlying Treatment Response to Deep Brain Stimulation Targeting the Inferior Thalamic Peduncle in Obsessive-Compulsive Disorder. Stereotact Funct Neurosurg. 2022;100(4):236-243. doi: 10.1159/000523826. Epub 2022 Apr 1. PMID: 35367990.
Difficult to Treat Chronic Pain Syndromes: How I do it with Neuromodulation
Thurs., June 6, 2024


Moderators:
Marc Russo, MBBS DA (UK) FANZCA, FFPMFANZCA and Sarah Love-Jones, BSC, MBBS, FRCA, FFPMRCA, EDPM
Topics and Faculty:
1) Neuromodulation for CRPS - Nadia Kriek, MD
2) Neuromodulation for Post-Herpetic Neuralgia - Nick Boulis, MD
3) Neuromodulation for Intractable Pelvic Pain - Corey Hunter, MD
Background Articles:
Hunter CW, Falowski S. Neuromodulation in Treating Pelvic Pain. Curr Pain Headache Rep. 2021 Feb 3;25(2):9. doi: 10.1007/s11916-020-00927-y. PMID: 33534006.
Kriek N, Groeneweg JG, Stronks DL, de Ridder D, Huygen FJ. Preferred frequencies and waveforms for spinal cord stimulation in patients with complex regional pain syndrome: A multicentre, double-blind, randomized and placebo-controlled crossover trial. Eur J Pain. 2017 Mar;21(3):507-519. doi: 10.1002/ejp.944. Epub 2016 Oct 7. PMID: 27714945.
Deogaonkar M, Slavin KV. Peripheral nerve/field stimulation for neuropathic pain. Neurosurg Clin N Am. 2014 Jan;25(1):1-10. doi: 10.1016/j.nec.2013.10.001. PMID: 24262894.
Texakalidis P, Tora MS, Boulis NM. Neurosurgeons' Armamentarium for the Management of Refractory Postherpetic Neuralgia: A Systematic Literature Review. Stereotact Funct Neurosurg. 2019;97(1):55-65. doi: 10.1159/000499476. Epub 2019 Apr 17. PMID: 30995653.
Statistics for Neuromodulation Research and Interpretation
Thurs. May 2, 2024


Moderators:
Rod Taylor, MSc, PhD and Lisa Goudman, PhD
Topics and Faculty:
1) Receiver Operating Characteristics and the Area Under the Curve - Alexander Thorpe, PhD 2) How to Interpret a Bayes Factor? - Quentin F. Gronau, PhD 3) What a P value can or cannot tell you - Garston Liang, PhD
Full Articles on INS website: Biostatistics in Neuromodulation Explained
- How to Interpret a Bayes Factor
- How to Interpret Risk Ratios, Odds Ratios and Hazard Ratios
- N-of-1 Trials & Their Use in Neuromodulation
- Types of Data and the Appropriate Tests for Them
- Receiver Operating Characteristics and the Area Under the Curve
- What a P-Value Can and Cannot Tell You
- The Fragility Index
By:
Quentin F. Gronau
Garston Liang
Alexander Thorpe
The Newcastle Cognition Lab
The University of Newcastle
Newcastle, NSW Australia
How to Develop a Successful Neuromodulation Practice: Advice from the Experts
Thurs., April 11, 2024
Visit the Member's Webinar Page for the recorded video and CME information.

Moderators:
Kiran Patel, MD and Christopher Gilligan, MD, MBA
Topics and Faculty:
1) Large Group Practice - Sean Li, MD, FIPP
2) Independent Practice- Jason Pope, MD
3) Academic Practice- Christopher Gilligan, MD, MBA
Background articles:
Darnall BD. The National Imperative to Align Practice and Policy with the Actual CDC Opioid Guideline. Pain Med. 2020 Feb 1;21(2):229-231. doi: 10.1093/pm/pnz152. PMID: 31334761.
Wang S, Polsunas P, Zhang C, Farrell ME, Clary AM, Dressler A, Engle AM, Giedraitis A, McDermott S, Hickey S, Zheng D, Brancolini S, Emerick T. Employment Contract Financial Models for the Pain Physician: A Primer. Pain Med. 2023 Apr 3;24(4):365-368. doi: 10.1093/pm/pnac143. PMID: 36165705.
Schwalb JM. Financial Sustainability of Neuromodulation for Pain. Neurosurg Clin N Am. 2022 Jul;33(3):281-286. doi: 10.1016/j.nec.2022.03.001. Epub 2022 May 25. PMID: 35718397.
State of the Art: Neuromodulation for Addiction Disorders
Thurs., March 7, 2024  Moderators:
Robert Levy, MD, PhD and Andres M. Lozano, OC, MD, PhD, FRCSC, FRSC, FCAHS
Topics and Faculty:
1) TMS, DBS and Other forms of Neuromodulation for Substance Use Disorders - Victor Tang, MD, MSc, FRCPC
2) Deep Brain Stimulation of the Nucleus Accumbens in the treatment of severe alcohol use disorder - Nir Lipsman, MD, PhD, FRCSC
3) Cortical Stimulation for the Treatment of Addictive Disorders - Dirk De Ridder, MD, PhD
Background Articles:
Davidson B, Giacobbe P, George TP, Nestor SM, Rabin JS, Goubran M, Nyman AJ, Baskaran A, Meng Y, Pople CB, Graham SJ, Tam F, Hamani C, Lipsman N. Deep brain stimulation of the nucleus accumbens in the treatment of severe alcohol use disorder: a phase I pilot trial. Mol Psychiatry. 2022 Oct;27(10):3992-4000. doi: 10.1038/s41380-022-01677-6. Epub 2022 Jul 21. PMID: 35858989.
Mehta, D.D., Praecht, A., Ward, H.B., Sanches, M., Sorkhou, M., Tang, V.M., Steele, V.R., Hanlon, C.A., and George, T.P. A systematic review and meta-analysis of neuromodulation therapies for substance use disorders. Neuropsychopharmacol. 49, 649–680 (2024). https://doi.org/10.1038/s41386-023-01776-0
De Ridder D, Perera S, Vanneste S. State of the Art: Novel Applications for Cortical Stimulation. Neuromodulation. 2017 Apr;20(3):206-214. doi: 10.1111/ner.12593. Epub 2017 Mar 28. PMID: 28371170.
Pelloux Y, Degoulet M, Tiran-Cappello A, Cohen C, Lardeux S, George O, Koob GF, Ahmed SH, Baunez C. Subthalamic nucleus high frequency stimulation prevents and reverses escalated cocaine use. Mol Psychiatry. 2018 Dec;23(12):2266-2276. doi: 10.1038/s41380-018-0080-y. Epub 2018 Jun 7. PMID: 29880881; PMCID: PMC8276917.
Third Generation Stimulation Paradigms for Spinal Cord Stimulation
Thurs., February 1, 2023
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators:
Robert Levy, MD, PhD and Marc Russo, MBBS DA (UK) FANZCA, FFPMFANZCA
Topics and Faculty:
1) Design of a Novel Third Generation SCS Paradigm - Michael Fishman, MD
2) Clinical Impact of a Novel Third Generation SCS Paradigm - Leo Kapural, MD, PhD
3) Integration of a Novel Third Generation SCS Paradigm with Real Time Patient Monitoring - Sean Li, MD
Background Articles:
Novel Spinal Cord Stimulation Waveforms for Treating Back and Leg Pain: A Systematic Review and Meta-Analysis of Randomized Controlled Trials Neuromodulation: Technology at the Neural Interface 26(5):905-916, 2023.
A novel, paresthesia-free spinal cord stimulation waveform for chronic neuropathic low back pain: six-month results of a prospective, single arm, dose-response study Russo, M, et al. Neuromodulation: Technology at the Neural Interface 26(7):1412-1423, 2023.
A Novel Pulsed Stimulation Pattern in Spinal Cord Stimulation: Clinical Results and Postulated Mechanisms of Action in the Treatment of Chronic Low Back and Leg Pain Desai, M, et al Neuromodulation: Technology at the Neural Interface 26(1):182-191, 2023.
This webinar has been sponsored by an educational grant from Biotronik.
Low Intensity Focused Ultrasound Neuromodulation
Thurs., December 7, 2023 Visit the Member's Webinar Page for the recorded video and CME information.
Moderators:
Julie Pilitsis, MD, PhD and Robert Chen, MA, MBBChir, MSc, FRCPC
Topics and Faculty:
1) Potential Mechanisms Supporting Low Intensity Focused Ultrasound for Neuromodulation - Martin M Monti, PhD
2) Low Intensity Focused Ultrasound for Epilepsy - Emma Lescrauwaet, PhD (c)
3) Low Energy Focused Ultrasound Neuromodulation for PNS and SCS - Julie Pilitsis, MD, PhD
Background Articles:
1) Dell'Italia J, Sanguinetti JL, Monti MM, Bystritsky A, Reggente N. Current State of Potential Mechanisms Supporting Low Intensity Focused Ultrasound for Neuromodulation. Front Hum Neurosci. 2022 Apr 25;16:872639. doi: 10.3389/fnhum.2022.872639. PMID: 35547195; PMCID: PMC9081930 - TBC.
2) Lescrauwaet E, Vonck K, Sprengers M, Raedt R, Klooster D, Carrette E, Boon P. Recent Advances in the Use of Focused Ultrasound as a Treatment for Epilepsy. Front Neurosci. 2022 Jun 20;16:886584. doi: 10.3389/fnins.2022.886584. PMID: 35794951; PMCID: PMC9251412. - Emma Lescrauwaet
3) Prabhala T, Hellman A, Walling I, Maietta T, Qian J, Burdette C, Neubauer P, Shao M, Stapleton A, Thibodeau J, Pilitsis JG. External focused ultrasound treatment for neuropathic pain induced by common peroneal nerve injury. Neurosci Lett. 2018 Sep 25;684:145-151. doi: 10.1016/j.neulet.2018.07.037. Epub 2018 Jul 26. PMID: 30056105. - Julie Pilitsis, MD, PhD
Peripheral Nerve Stimulation for Chronic Pain
Thurs., November 2, 2023
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators:
Konstantin V. Slavin, MD and Christopher Winfree, MD
Topics and Faculty:
1) Systematic Review of Peripheral Nerve Stimulation for Chronic Pain- Jay Grider, DO, PhD, MBA
2) Temporary Peripheral Nerve Stimulation for Chronic Pain- Christine Hunt, DO
3) Advances in Neuromodulation in the Oncologic Population- Amitabh Gulati, MD, FIPP, CIPS, ASRA-PMUC
4) Ultrasound-Guided Temporary Peripheral Nerve Stimulation of Spinal Nerves for Dermatomal Pain- Ojas Mainkar, MD
Background articles:
Deer TR, Esposito MF, McRoberts WP, Grider JS, Sayed D, Verrills P, Lamer TJ, Hunter CW, Slavin KV, Shah JM, Hagedorn JM, Simopoulos T, Gonzalez DA, Amirdelfan K, Jain S, Yang A, Aiyer R, Antony A, Azeem N, Levy RM, Mekhail N. A Systematic Literature Review of Peripheral Nerve Stimulation Therapies for the Treatment of Pain. Pain Med. 2020 Aug 1;21(8):1590-1603. doi: 10.1093/pm/pnaa030. PMID: 32803220.
Mainkar O, Solla CA, Chen G, Legler A, Gulati A. Pilot Study in Temporary Peripheral Nerve Stimulation in Oncologic Pain. Neuromodulation. 2020 Aug;23(6):819-826. doi: 10.1111/ner.13139. Epub 2020 Mar 17. PMID: 32185844; PMCID: PMC7496167.
Mainkar O, Solla CA, Chen G, Legler A, Gulati A. Pilot Study in Temporary Peripheral Nerve Stimulation in Oncologic Pain. Neuromodulation. 2020 Aug;23(6):819-826. doi: 10.1111/ner.13139. Epub 2020 Mar 17. PMID: 32185844; PMCID: PMC7496167.
Mainkar O, Singh H, Gargya A, Lee J, Valimahomed A, Gulati A. Ultrasound-Guided Peripheral Nerve Stimulation of Cervical, Thoracic, and Lumbar Spinal Nerves for Dermatomal Pain: A Case Series.Neuromodulation. 2021 Aug;24(6):1059-1066. doi: 10.1111/ner.13334. Epub 2020 Dec 14. PMID: 33314509.
This webinar was supported by an educational grant from SPR Therapeutics.
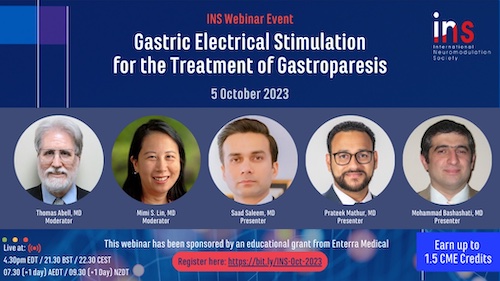
Gastric Electrical Stimulation for the Treatment of Gastroparesis
Thurs., October 5, 2023
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators:
Thomas Abell, M.D and Mimi S. Lin, M.D
Topics and Faculty:
1) Gastric Electrical Stimulation for the Treatment of Gastroparesis or Gastroparesis-like Symptoms: A Systematic Review and Meta-analysis- Saad Saleem MD
2) Baseline Predictive Factors for Foregut and Hindgut Response to Long-term Gastric Electrical Stimulation - Prateek Mathur MD
3) Gastric Electrical Stimulation for Treatment of Refractory Gastroparesis: The Current Approach to Management- Mohammad Bashashati MD
Background articles:
1) Saleem S, Aziz M, Khan AA, Williams MJ, Mathur P, Tansel A, Barber A, Abell TL. Gastric Electrical Stimulation for the Treatment of Gastroparesis or Gastroparesis-like Symptoms: A Systemic Review and Meta-analysis. Neuromodulation. 2022 Dec 2:S1094-7159(22)01338-1. doi: 10.1016/j.neurom.2022.10.048. Epub ahead of print. PMID: 36464562.
2) Elmasry M, Hassan H, Mathur P, Stocker A, Atassi H, Saleem S, McElmurray L, Cooper K, Hughes MG, Starkebaum W, Pinkston C, Abell T. Baseline predictive factors for foregut and hindgut response to long-term gastric electrical stimulation using augmented energy. Neurogastroenterol Motil. 2022 Jun;34(6):e14274. doi: 10.1111/nmo.14274. Epub 2021 Oct 26. PMID: 34697860.
3) Shanker A, Bashashati M, Rezaie A. Gastric Electrical Stimulation for Treatment of Refractory Gastroparesis: the Current Approach to Management. Curr Gastroenterol Rep. 2021 Jan 22;23(2):2. doi: 10.1007/s11894-020-00803-0. PMID: 33483775; PMCID: PMC7822763.
This webinar was supported by an educational grant from Enterra Medical.
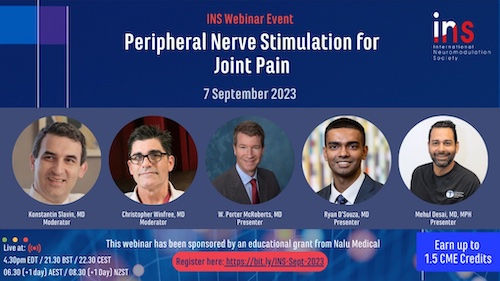
Peripheral Nerve Stimulation for Joint Pain
Thurs., September 7, 2023 Visit the Member's Webinar Page for the recorded video and CME information.
Moderators:
Christopher Winfree, MD and Konstantin Slavin, MD
Topics and Faculty:
1) Peripheral Stimulation of the Saphenous and Superior Lateral Geniculate Nerves for Chronic Knee Pain - W. Porter McRoberts, MD
2) Evidence-Based Clinical Guidelines from the American Society of Pain and Neuroscience for the Use of Implantable Peripheral Nerve Stimulation in the Treatment of Chronic Pain - Ryan D'Souza, MD
3) Axillary Peripheral Nerve Stimulation for Chronic Shoulder Pain- Mehul Desai, MD, MPH
Background articles:
1) Hasoon J, Chitneni A, Urits I, Viswanath O, Kaye AD. Peripheral Stimulation of the Saphenous and Superior Lateral Genicular Nerves for Chronic Knee Pain. Cureus. 2021 Apr 29;13(4):e14753. doi: 10.7759/cureus.14753. PMID: 34084679; PMCID: PMC8163353.
2) Mazzola A, Spinner D. Ultrasound-Guided Peripheral Nerve Stimulation for Shoulder Pain: Anatomic Review and Assessment of the Current Clinical Evidence. Pain Physician. 2020 Sep;23(5):E461-E474. PMID: 32967397.
3) Mansfield JT, Desai MJ. Axillary Peripheral Nerve Stimulation for Chronic Shoulder Pain: A Retrospective Case Series. Neuromodulation. 2020 Aug;23(6):812-818. doi: 10.1111/ner.13096. Epub 2020 Jan 13. PMID: 31930660.
This webinar was supported by an educational grant from Nalu Medical.
Significance of Remote Monitoring of Implanted Electrical Devices:
What Neuromodulation Can Learn from Cardiac Modulation
Thurs., July 6, 2023
Moderators:
Robert Levy, MD, PhD and Kiran Patel, MD
Presenters:
Peter Silburn, MD, PhD, Bruce L. Wilkoff, MD and David Slotwiner, MD, FHRS, FACC
Lectures:
1) A Primer on Remote Physiologic and Therapeutic Monitoring Codes - Peter Silburn, BSc, MBBS, PhD, FRACP
2) HRS/EHRA Expert Consensus on the Monitoring of Cardiovascular Implantable Electronic Devices (CIEDs): Description of Techniques, Indications, Personnel, Frequency and Ethical Considerations - Bruce L. Wilkoff, MD
3) HRS Expert Consensus Statement on Remote Interrogation and Monitoring for Cardiovascular Implantable Electronic Devices - David Slotwiner, MD, FHRS, FACC
Background articles:
1) Wilkoff BL, Auricchio A, Brugada J, Cowie M, Ellenbogen KA, Gillis AM, Hayes DL, Howlett JG, Kautzner J, Love CJ, Morgan JM, Priori SG, Reynolds DW, Schoenfeld MH, Vardas PE; Heart Rhythm Society; European Heart Rhythm Association; American College of Cardiology; American Heart Association; European Society of Cardiology; Heart Failure Association of ESC; Heart Failure Society of America. HRS/EHRA expert consensus on the monitoring of cardiovascular implantable electronic devices (CIEDs): description of techniques, indications, personnel, frequency and ethical considerations. Heart Rhythm. 2008 Jun;5(6):907-25. doi: 10.1016/j.hrthm.2008.04.013. PMID: 18551743.
2) Slotwiner D, Varma N, Akar JG, Annas G, Beardsall M, Fogel RI, Galizio NO, Glotzer TV, Leahy RA, Love CJ, McLean RC, Mittal S, Morichelli L, Patton KK, Raitt MH, Ricci RP, Rickard J, Schoenfeld MH, Serwer GA, Shea J, Varosy P, Verma A, Yu CM. HRS Expert Consensus Statement on remote interrogation and monitoring for cardiovascular implantable electronic devices. Heart Rhythm. 2015 Jul;12(7):e69-100.
doi: 10.1016/j.hrthm.2015.05.008. Epub 2015 May 14. PMID: 25981148.
3) Fozia Zahir Ahmed, Joanne K. Taylor, Caroline Green, Lucy Moore, Angelic Goode, Paula Black, Lesley Howard, Catherine Fullwood, Amir Zaidi, Alison Seed, Colin Cunnington, Manish Motwani. Triage-HF Plus: a novel device-based remote monitoring pathway to identify worsening heart failure. First published: 03 December 2019 https://doi.org/10.1002/ehf2.12529
This webinar was supported by an educational grant from BIOTRONIK.
Impact of Biological Sex on Spinal Cord Stimulation
Thurs., June 1, 2023
Moderators
Julie Pilitsis, MD, PhD and Erika Petersen, MD
Lectures
1) Impact of biological sex on the outcomes of spinal cord stimulation in patients with chronic pain - Shrif Costandi, MD
2) Men and Women Respond Equally Well to Spinal Cord and Dorsal Root Ganglion Stimulation - Sheila Black, FFPMRCA, FRCA, MB ChB
3) Sex-Specific Differences in the Efficacy of Traditional Low Frequency Versus High Frequency Spinal Cord Stimulation for Chronic Pain - Rosalynn R.Z. Conic MD, PhD, MPH
4) Less Pain Relief, More Depression, and Female Sex Correlate With Spinal Cord Stimulation Explants - Lisa Goudman, PhD
Background Articles
1) Mekhail N, Costandi S, Saweris Y, Armanyous S, Chauhan G. Impact of biological sex on the outcomes of spinal cord stimulation in patients with chronic pain. Pain Pract. 2022 Apr;22(4):432-439. doi: 10.1111/papr.13097. Epub 2021 Dec 9. PMID: 34845813.
2) Bretherton B, de Ridder D, Crowther T, Black S, Whelan A, Baranidharan G. Men and Women Respond Equally Well to Spinal Cord and Dorsal Root Ganglion Stimulation. Neuromodulation. 2022 Oct;25(7):1015-1023. doi: 10.1111/ner.13484. Epub 2022 Jun 14. PMID: 34156722.
3) Conic RRZ, Caylor J, Cui CL, Reyes Z, Nelson E, Yin S, Lerman I. Sex-specific differences in the efficacy of traditional low frequency versus high frequency spinal cord stimulation for chronic pain. Bioelectron Med. 2022 Apr 28;8(1):8. doi: 10.1186/s42234-022-00090-2. PMID: 35484578; PMCID: PMC9052649.
4) Slyer J, Scott S, Sheldon B, Hancu M, Bridger C, Pilitsis JG. Less Pain Relief, More Depression, and Female Sex Correlate With Spinal Cord Stimulation Explants. Neuromodulation. 2020 Jul;23(5):673-679. doi: 10.1111/ner.13036. Epub 2019 Aug 19. PMID: 31429165.
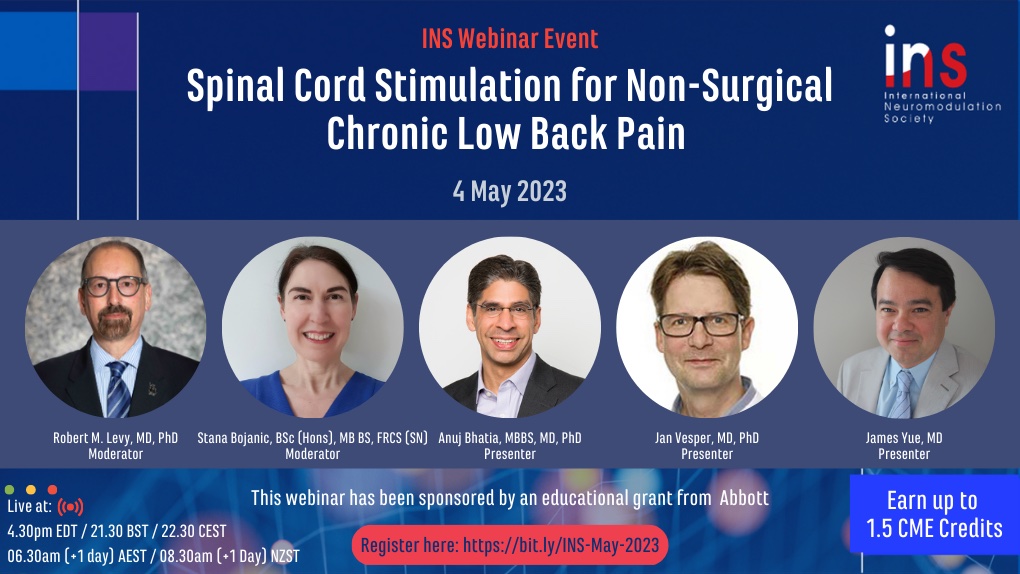
Spinal Cord Stimulation for Non-Surgical Chronic Low Back Pain
Thurs., May 4 2023
Moderators
Robert Levy, MD, PhD and Stana Bojanic, BSc (Hons), MB BS, FRCS [SN]
Lectures
Systematic Literature Review of Spinal Cord Stimulation in Patients with Chronic Back Pain Without Prior Surgery - Anuj Bhatia, MBBS, MD, PhD
Neurostimulation is an Effective Treatment Option for Chronic Back Pain Regardless of Prior Spinal Surgery - Jan Vesper, MD, PhD
Results of a Large Scale Randomized Controlled Trial Evaluating SCS Versus Conventional Management of Nonsurgical Chronic Low Back Pain - James Yue, MD
Background Articles
1) Eckermann JM, Pilitsis JG, Vannaboutathong C, Wagner BJ, Province-Azalde R, Bendel MA. Systematic Literature Review of Spinal Cord Stimulation in Patients With Chronic Back Pain Without Prior Spine Surgery. Neuromodulation. 2021 Aug 18. doi: 10.1111/ner.13519. Epub ahead of print. PMID: 34407288.
2) Hagedorn J, Vesper J, Falowski S, Heros R, Papa A, Jannu A, Mansouri M, O084 / #701 Neurostimulation is an Effective Treatment Option for Chronic Back Pain Regardless of Prior Spinal Surgery: Track 3: Neurostimulation for Back and Leg Pain. INS 15th World Congress Abstracts. 21-26 May 2022, Barcelona, Spain. Neuromodulation, Volume 25, Issue 7 Supplement, 2022, Pages S1-S374. doi: 10.1016/j.neurom.2022.08.122
3) Yue JJ, Gilligan CJ, Falowski S, Jameson J, Desai MJ, Moeschler S, Pilitsis J, Heros R, et al. 226. Surgical Treatment of Refractory Low Back Pain using Implanted BurstDR Spinal Cord Stimulation (SCS) in a Cohort of Patients without Options for Corrective Surgery: Findings and Results from the DISTINCT Study, a Prospective Randomized Multi-center Controlled Trial, The Spine Journal, Volume 22, Issue 9, Supplement, 2022, Pages S120-S121, ISSN 1529-9430, https://doi.org/10.1016/j.spinee.2022.06.246.
This webinar was supported by an educational grant from Abbott.
Closed Loop Vagus Nerve Stimulation for Drug Resistant Epilepsy
Thurs., April 6, 2023
Moderators
Kristl Vonck, MD, PhD and Arthur Cukiert, MD, PhD
Lectures
Seizure Improvement Following Vagus Nerve Stimulator (VNS) Battery Change with Cardiac-Based Seizure Detection Automatic Stimulation: Early Experience in a Regional Paediatric Unit - William B. Lo, MBBChir FRCS FEBNS
Comparison of Traditional and Closed Loop Vagus Nerve Stimulation for Treatment of Pediatric Drug-Resistant Epilepsy: A Propensity-Matched Retrospective Cohort Study - Nallammai Muthiah, BS
Impact of Cardiac-Based Vagus Nerve Stimulation Closed-Loop Stimulation on the Seizure Outcome of Patients with Generalized Epilepsy: A Prospective, Individual-Control Study - Arthur Cukiert, MD, PhD
Background Articles
1) Lo WB, Chevill B, Philip S, Agrawal S, Walsh AR. Seizure improvement following vagus nerve stimulator (VNS) battery change with cardiac-based seizure detection automatic stimulation (AutoStim): early experience in a regional paediatric unit. Childs Nerv Syst. 2021 Apr;37(4):1237-1241. doi: 10.1007/s00381-020-04962-3. Epub 2020 Nov 10. PMID: 33174154.
2) Muthiah N, Akwayena E, Vodovotz L, Sharma N, Jeong JH, White GE, Abel TJ. Comparison of traditional and closed loop vagus nerve stimulation for treatment of pediatric drug-resistant epilepsy: A propensity-matched retrospective cohort study. Seizure. 2022 Jan;94:74-81. doi: 10.1016/j.seizure.2021.11.016. Epub 2021 Nov 29. PMID: 34872020.
3) Cukiert A, Cukiert CM, Mariani PP, Burattini JA. Impact of Cardiac-Based Vagus Nerve Stimulation Closed-Loop Stimulation on the Seizure Outcome of Patients With Generalized Epilepsy: A Prospective, Individual-Control Study. Neuromodulation. 2021 Aug;24(6):1018-1023. doi: 10.1111/ner.13290. Epub 2020 Oct 12. PMID: 33047437.
This webinar was supported by a grant from LivaNova.
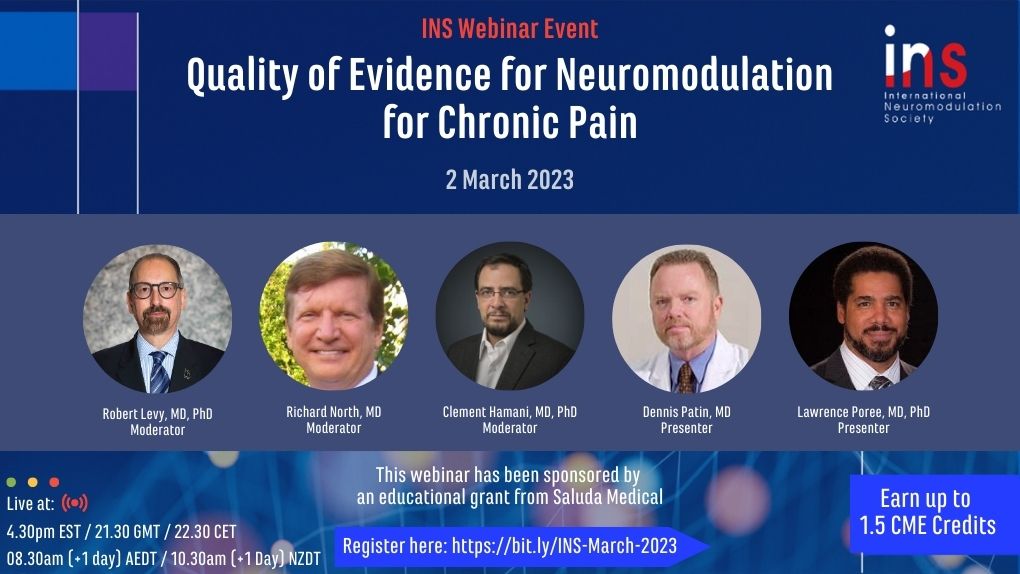
Quality of Evidence for Neuromodulation for Chronic Pain
Thurs., March 2, 2023
Moderators
Robert M. Levy, MD, PhD and Richard North, MD
Lectures
Quality of Contemporary Evidence for Spinal Cord Stimulation for Chronic Pain – Clement Hamani, MD, PhD
Quality of Evidence for Neuromodulation for Focal Neuropathic Pain: Dorsal Root Ganglion, 10K High Frequency and Burst Spinal Cord Stimulation – Dennis Patin, MD
Superiority of Holistic Outcome Measures as Compared to Pain Measures Alone in Studies of SCS for Chronic Pain: Validation and Application in a Randomized, Controlled Trial of Spinal Cord Stimulation for Chronic Pain – Lawrence Poree, MD, PhD, MPH
Background Articles
1) Knotkova H, Hamani C, Sivanesan E, Le Beuffe MFE, Moon JY, Cohen SP, Huntoon MA. Neuromodulation for chronic pain. Lancet. 2021 May 29;397(10289):2111-2124. doi: 10.1016/S0140-6736(21)00794-7. PMID: 34062145.
2) Podgorski Iii E, Mascaro P, Patin D. Comparison of FDA-Approved Electrical Neuromodulation Techniques for Focal Neuropathic Pain: A Narrative Review of DRG, HF10, and Burst Neuromodulation. Pain Physician. 2021 Jul;24(4):E407-E423. PMID: 34213866.
3) Levy RM, Mekhail N, Abd-Elsayed A, Abejón D, Anitescu M, Deer TR, Eldabe S, Goudman L, Kallewaard JW, Moens M, Petersen EA, Pilitsis JG, Pope JE, Poree L, Raslan AM, Russo M, Sayed D, Staats PS, Taylor RS, Thomson S, Verrills P, Duarte RV. Holistic Treatment Response: An International Expert Panel Definition and Criteria for a New Paradigm in the Assessment of Clinical Outcomes of Spinal Cord Stimulation. Neuromodulation. 2023 Jan 3:S1094-7159(22)01379-4. doi: 10.1016/j.neurom.2022.11.011. Epub ahead of print. PMID: 36604242.
This webinar has been supported by a grant from Saluda Medical.
Clinical Trials in Spinal Cord Stimulation - Current Status
Thurs., Feb. 2, 2023
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Konstantin Slavin, MD and Julie Pilitsis, MD, PhD
Lectures
Randomized Placebo-/Sham-Controlled Trials of Spinal Cord Stimulation: A Systematic Review and Methodological Appraisal – Rod Taylor, PhD
Systematic Review and Meta-Analysis of Placebo/Sham Controlled Randomised Trials of Spinal Cord Stimulation for Neuropathic Pain – Richard North, MD
Background Articles
1) Carron R, Roncon P, Lagarde S, Dibué M, Zanello M, Bartolomei F. Latest Views on the Mechanisms of Action of Surgically Implanted Cervical Vagal Nerve Stimulation in Epilepsy. Neuromodulation. 2022 Sep 1:S1094-7159(22)01222-3. doi: 10.1016/j.neurom.2022.08.447. Epub ahead of print. PMID: 36064522.
2) Russo A, Hyslop A, Gentile V, Chiarello D, Messana T, Miller I, Zucchelli M, Lima M, Ragheb J, Pini A, Cordelli DM, Resnick T, Jayakar P, Duchowny M. Early Implantation as a Main Predictor of Response to Vagus Nerve Stimulation in Childhood-Onset Refractory Epilepsy. J Child Neurol. 2021 Apr;36(5):365-370. doi: 10.1177/0883073820974855. Epub 2020 Nov 25. PMID: 33236677.
3) Santhumayor B, Karkare S, Kothare S, Rodgers S. Evaluating vagus nerve stimulation treatment with heart rate monitoring in pediatric patients with intractable epilepsy. Childs Nerv Syst. 2022 Mar;38(3):547-556. doi: 10.1007/s00381-021-05416-0. Epub 2021 Nov 27. PMID: 34837500.
4) Zhang L, Hall M, Lam SK. Hospital costs associated with vagus nerve stimulation and medical treatment in pediatric patients with refractory epilepsy. Epilepsia. 2022 May;63(5):1141-1151. doi: 10.1111/epi.17208. Epub 2022 Mar 13. PMID: 35188675; PMCID: PMC9311159.
This webinar has been supported by a grant from Nevro.
Recent Updates on Vagus Nerve Stimulation in the Pediatric Population
Thurs., Jan. 5, 2023
Visit the Member's Webinar Page for the recorded video and CME information.

Moderators
Arthur Cukiert, MD, PhD and George Ibrahim, MD, PhD
Lectures
Latest Views on the Mechanisms of Action of Surgically Implanted Cervical Vagal Nerve Stimulation in Epilepsy - Romain Carron, MD, PhD
Evaluating vagus nerve stimulation treatment with heart rate monitoring in pediatric patients with intractable epilepsy. Child's nervous system - Brandon Santhumayor, MD
Hospital costs associated with vagus nerve stimulation and medical treatment in pediatric patients with refractory epilepsy - Sandi Lam, MD, MBA
Background Articles
1) Carron R, Roncon P, Lagarde S, Dibué M, Zanello M, Bartolomei F. Latest Views on the Mechanisms of Action of Surgically Implanted Cervical Vagal Nerve Stimulation in Epilepsy. Neuromodulation. 2022 Sep 1:S1094-7159(22)01222-3. doi: 10.1016/j.neurom.2022.08.447. Epub ahead of print. PMID: 36064522.
2) Russo A, Hyslop A, Gentile V, Chiarello D, Messana T, Miller I, Zucchelli M, Lima M, Ragheb J, Pini A, Cordelli DM, Resnick T, Jayakar P, Duchowny M. Early Implantation as a Main Predictor of Response to Vagus Nerve Stimulation in Childhood-Onset Refractory Epilepsy. J Child Neurol. 2021 Apr;36(5):365-370. doi: 10.1177/0883073820974855. Epub 2020 Nov 25. PMID: 33236677.
3) Santhumayor B, Karkare S, Kothare S, Rodgers S. Evaluating vagus nerve stimulation treatment with heart rate monitoring in pediatric patients with intractable epilepsy. Childs Nerv Syst. 2022 Mar;38(3):547-556. doi: 10.1007/s00381-021-05416-0. Epub 2021 Nov 27. PMID: 34837500.
4) Zhang L, Hall M, Lam SK. Hospital costs associated with vagus nerve stimulation and medical treatment in pediatric patients with refractory epilepsy. Epilepsia. 2022 May;63(5):1141-1151. doi: 10.1111/epi.17208. Epub 2022 Mar 13. PMID: 35188675; PMCID: PMC9311159.
This webinar has been supported by an educational grant from LivaNova.
Artificial Intelligence and Computational Modeling in Spinal Cord Stimulation:
State of the Art Basic and Applied Research
Thurs., Dec. 1, 2022
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert Levy, MD, PhD and Cecile de Vos, PhD
Lectures
Surround Inhibition: A New Potential Spinal Cord Stimulation Mechanisms of Action - Warren Grill, PhD
Artificial Intelligence-Driven SCS: Early Patient Feedback on Personalized Therapy Recommendations - Richard Rauck, MD
Integrating Artificial Intelligence and Spinal Cord Stimulation in the Treatment of Chronic Pain - Jeff Rogers, PhD
Background Articles
1) Titus, N.D., Gilbert, J.E., Grill, W.M. (2021). Biophysics and Mechanisms of Spinal Cord Stimulation for Chronic Pain. Thakor, N.V. (eds) Handbook of Neuroengineering. Springer, Singapore. https://doi.org/10.1007/978-981-15-2848-4_99-2
2) Rauck, Richard L., et al. A Prospective Global Registry of Real-world Outcomes Using Spinal Cord Stimulation Systems for Chronic Pain. AAPM 2019 Annual Meeting Abstracts, Pain Medicine, Volume 20, Issue 3, March 2019, Pages 583–660, https://doi.org/10.1093/pm/pny317
3) Rauck R, Berger S, Cecchi G, Agurto C, Eyigoz E, Lechleiter K, Huynh D, Brad Hershey, Loudermilk E, Paez J, Bojrab L, Noles J, Turley T, Ibrahim M, Patwardhan A, Scowcroft J, Rene Przkora, Miller N, Chaiban G, Matt McDonald, Rogers J. ID:15982 Chronic Pain Patients During COVID-19: Machine Learning Reveals Attributes Leading to Pandemic Susceptibility and Resilience. Neuromodulation. 2022 Jun;25(4):S27–9. https://doi.org/10.1016/j.neurom.2022.02.160
This webinar has been supported by an educational grant from Boston Scientific.
Socioeconomic Disparity in Spinal Cord Stimulation
Thurs., Nov. 3, 2022
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Stephanie Vanterpool, MD, MBA and Erika Petersen, MD
Lectures
Racial and Socioeconomic Disparities in Spinal Cord Stimulation Among the Medicare Population - Charles Odonkor, MD, MA
Socioeconomic Disparities in the Utilization of Spinal Cord Stimulation Therapy in Patients with Chronic Pain - Thomas Simopoulous, MD
Demographic Trends in Paddle Lead Spinal Cord Stimulator Placement: Private Insurance and Medicare Beneficiaries - Vwaire Orhurhu, MD, MPH
Racism in Pain Medicine and Neuromodulation: We Can and Should Do More? - Natalie Strand, MD
Background Articles
Jones MR, Orhurhu V, O'Gara B, Brovman EY, Rao N, Vanterpool SG, Poree L, Gulati A, Urman RD. Racial and Socioeconomic Disparities in Spinal Cord Stimulation Among the Medicare Population. Neuromodulation. 2021 Apr;24(3):434-440. doi: 10.1111/ner.13373. Epub 2021 Mar 15. PMID: 33723896.
Odonkor CA, Tucker-Bartley A, Leitner B, Chude C, Hirani S, Poree L. Closing the gap in representation of racial and ethnic minorities in pain medicine: A 2018-2019 status report. J Natl Med Assoc. 2022 Jan;113(6):612-615. doi: 10.1016/j.jnma.2021.05.010. Epub 2021 Jun 18. PMID: 34148658.
Labaran L, Bell J, Puvanesarajah V, Jain N, Aryee JN, Raad M, Jain A, Carmouche J, Hassanzadeh H. Demographic Trends in Paddle Lead Spinal Cord Stimulator Placement: Private Insurance and Medicare Beneficiaries. Neurospine. 2020 Jun;17(2):384-389. doi: 10.14245/ns.1938276.138. Epub 2020 Feb 1. PMID: 32054146; PMCID: PMC7338957.
Strand NH, Mariano ER, Goree JH, Narouze S, Doshi TL, Freeman JA, Pearson ACS. Racism in Pain Medicine: We Can and Should Do More. Mayo Clin Proc. 2021 Jun;96(6):1394-1400. doi: 10.1016/j.mayocp.2021.02.030. PMID: 34088411.
Update on Peripheral Nerve Stimulation
Thurs., Oct. 6, 2022
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Christopher Winfree, MD and Lawrence Poree, MD, PhD
Topics and Faculty
Peripheral Nerve Stimulation in Pain Management: A Systematic Review - Krishnan Chakravarthy, MD, PhD
Sciatic, Femoral and Lateral Femoral Cutaneous Nerve Ultrasound-Guided Peripheral Nerve Stimulation - Amitabh Gulati, MD
Peripheral Nerve Stimulation for the 21st Century: Sural, Superficial Peroneal and Tibial Nerves - Scott Pritzlaff, MD
Background Articles
1) Xu J, Sun Z, Wu J, Rana M, Garza J, Zhu AC, Chakravarthy KV, Abd-Elsayed A, Rosenquist E, Basi H, Christo P, Cheng J. Peripheral Nerve Stimulation in Pain Management: A Systematic Review. Pain Physician. 2021 Mar;24(2), E131-E152. PMID: 33740342; PMCID: PMC8897810.
2) Singh H, Gargya A, Lin T, Gulati A. Sciatic, Femoral, and Lateral Femoral Cutaneous Nerve Ultrasound-Guided Percutaneous Peripheral Nerve Stimulation. Pain Med. 2020 Aug 1;21(Suppl 1):S47-S50. doi: 10.1093/pm/pnaa040. PMID: 32804221; PMCID: PMC7828577.
3) Gofeld M, Agur A. Peripheral Nerve Stimulation for Chronic Shoulder Pain: A Proof of Concept Anatomy Study. Neuromodulation. 2018 Apr;21(3):284-289. doi: 10.1111/ner.12749. Epub 2018 Jan 3. PMID: 29314501.
4) Hanyu-Deutmeyer A, Pritzlaff SG. Peripheral Nerve Stimulation for the 21st Century: Sural, Superficial Peroneal, and Tibial Nerves. Pain Med. 2020 Aug 1;21(Suppl 1):S64-S67. doi: 10.1093/pm/pnaa202. PMID: 32804232.
This webinar has been supported by an educational grant from Nalu Medical.
Spinal Cord Stimulation for Nociceptive Pain
Thurs., Sept. 1, 2022
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert Levy, MD, PhD and Stana Bojanic BSc (Hons), MB BS, FRCS (SN)
Topics and Faculty
Current Perspectives on Spinal Cord Stimulation for the Treatment of Cancer Pain: Does this Include Mixed Nociopathic Pain and/or Nociceptive Pain? – Jonathan Hagedorn, MD
Effects of Dorsal Column Spinal Cord Stimulation on Neuroinflammation: Molecular Mechanisms and Clinical Outcomes: Does this Data Warrant Consideration of SCS for Nociceptive Pain? – Krishnan Chakravarthy, MD, PhD
Spinal Cord Stimulation for Visceral Pain: Is this SCS Success for a Nociceptive Pain Syndrome? – Maynak Gupta, MD
Background Articles
1) Hagedorn JM, Pittelkow TP, Hunt CL, D'Souza RS, Lamer TJ. Current Perspectives on Spinal Cord Stimulation for the Treatment of Cancer Pain. J Pain Res. 2020 Dec 7;13:3295-3305. doi: 10.2147/JPR.S263857. PMID: 33324090; PMCID: PMC7732175.
2) Echeverria-Villalobos M, Mitchell J, Fiorda-Diaz J, Weaver T. Effects of Dorsal Column Spinal Cord Stimulation on Neuroinflammation: Revisiting Molecular Mechanisms and Clinical Outcomes on Chronic Lumbar/Leg Pain and Failed Back Surgery Syndrome. J Pain Res. 2021 Jul 30;14:2337-2345. doi: 10.2147/JPR.S309872. PMID: 34354373; PMCID: PMC8331196.
3) Woodroffe RW, Pearson AC, Pearlman AM, Howard MA, Nauta HJW, Nagel SJ, Hori YS, Machado AG, Almeida Frizon L, Helland L, Holland MT, Gillies GT, Wilson S. Spinal Cord Stimulation for Visceral Pain: Present Approaches and Future Strategies. Pain Med. 2020 Oct 1;21(10):2298-2309. doi: 10.1093/pm/pnaa108. PMID: 32719876.
The Neurostimulation Appropriateness Consensus Committee (NACC): Recommendations on Best Practices for Cervical Neurostimulation
Thurs. July 7, 2022
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert M. Levy, MD, PhD, and Timothy Deer, MD
Topics and Faculty
The NACC Process – Timothy Deer, MD
Anatomic Considerations/Imaging – Marc Russo, MBBS DA (UK), FANZCA, FFMANZCA
Surgical Techniques (Including Percutaneous and Paddle Leads) – Giancarlo Barolat, MD
Dorsal Root Ganglion Stimulation in the Cervical Region – Kiran Patel, MD
Risk Mitigation and Complication Management – David Provenzano, MD
Neurostimulation for Diabetes and Its Complications
Thurs. June 2, 2022
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert M. Levy, MD, PhD, and Erika Petersen, MD
Topics and Faculty
Retrospective Case Series on the Treatment of Painful Diabetic Peripheral Neuropathy With Dorsal Root Ganglion Stimulation – Jan Vesper, MD, PhD
SCS for the Management of Painful Diabetic Neuropathy: A Systematic Review and Metanalysis of Aggregate Patient Data – Ashish Gulve, FRCA, FFPMRCA, FFPMCAI,DPMed, FCARCSI, MD, MBBS
Effect of High-frequency Spinal Cord Stimulation in Patients with Painful Diabetic Neuropathy: A Randomized Clinical Trial – Erika Petersen, MD
This webinar has been supported by an educational grant from Nevro
The Neurostimulation Appropriateness Consensus Committee (NACC):
Recommendations for Surgical Technique for Spinal Cord Stimulation
Thurs. May 5, 2022
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert Levy, MD, PhD, and Marc Russo, MBBS
Topics and Faculty
Preoperative Assessment and Considerations (Including Antibiotics and Antithrombotics) – Marc Russo, MBBS
Surgical Techniques (Including Percutaneous and Paddle Leads) – Philippe Rigoard, MD, PhD
Wound Closure and Postoperative Care – Stana Bojanic, MBBS
Complication Management – Jonathan Hagedorn, MD
Vagus Nerve Stimulation: Impact on Cognition and Depression
Thurs. April 7, 2022
Visit the Member's Webinar Page for the recorded video and CME information.
Topics and Faculty
Depression and Cognitive Dysfunction in Chronic Epilepsy Patients - Jukka Peltola, MD, PhD
Vagus Nerve Stimulation for Depression - Charles Conway, MD
Vagus Nerve Stimulation for Cognitive Dysfunction - Harold Sackeim, MD
This webinar has been supported by an educational grant from LivaNova
Closed Loop Deep Brain Stimulation
Thurs. March 3, 2022
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Konstantin Slavin, MD and Jan Vesper, MD, PhD
Faculty and Topics
Neurochemical and Electrophysiological Measurements for Closed Loop DBS – Kendall Lee, MD, PhD
Closed Loop DBS Controller Technology – Warren Grill, PhD
Dual Threshold Closed-Loop DBS in Parkinson’s Disease – Helen Bronte-Stewart, MD
This webinar was supported by an educational grant from Medtronic. Medtronic was not involved in the creation or delivery of any program content and does not control whether the materials conform to FDA approved or cleared indications.
Novel Stimulation Paradigms for SCS – Second Generation
Thurs. Feb. 3, 2022
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert M. Levy, MD, PhD, and Cecile de Vos, PhD
Faculty and Topics
Differential Target Multiplexed Spinal Cord Stimulation – Ricardo Vallejo, MD, PhD
A Novel Pulsed Stimulation Pattern for SCS Pain Management – Lawrence Poree, MD, PhD
An Update on Closed Loop Spinal Cord Stimulation – Marc Russo, MBBS DA (UK) FANZCA FFPMANZCA
This webinar has been supported by an educational grant from Medtronic.
Salvage Therapies for Failed Spinal Cord Stimulation
Thurs. Jan. 6, 2022
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert M. Levy, MD, PhD and Dirk De Ridder, MD, PhD
Faculty and Topics
Differential Diagnosis of Loss of Treatment Effect with SCS – Jonathan Carlson, MD
Approaches to Failure of SCS Therapy Using Novel SCS Waveforms –Krishnan Chakravarthy, MD, PhD
Approaches to Failure of SCS Therapy Using Dorsal Root Ganglion Stimulation – Corey Hunter, MD
This webinar has been supported by an educational grant from Abbott.
Issues with Implanted Batteries for Neuromodulation
Thurs. Dec.. 2, 2021
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert M. Levy, MD, PhD and Julie Pilitsis, MD, PhD
Faculty and Topics
Issues with Implantable Batteries for SCS/PNS - Richard North, MD
Novel Non-Implanted Battery Options and Technique for SCS - Lawrence Poree, MD, PhD
Novel Non-Implanted Battery Options and Technique for PNS - Dawood Sayed, MD
This webinar has been supported by an educational grant from Nalu Medical.
Closed Loop Spinal Cord Stimulation
Thursday, Nov. 4, 2021
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Marc Russo, MBBS DA (UK) FANZCA FFPMANZCA and Stana Bojanic, BSc (Hons), MB BS, FRCS (SN)
Faculty and Topics
Unmet Needs of Current Spinal Cord Stimulation Systems – Sean Li, MD
Closed-Loop Spinal Cord Stimulation using Real-Time Evoked Compound Action Potential Control – Marc Russo, MBBS DA (UK) FANZCA FFPMANZCA
Real-time Evoked Compound Action Potential Controlled Closed-Loop Spinal Cord Stimulation: 24-month Outcomes of Clinical Trial – Lawrence Poree, MD, PhD, MPH
Background
Mekhail N, Levy RM, Deer TR, Kapural L, Li S, Amirdelfan K, Hunter CW, Rosen SM, Costandi SJ, Falowski SM, Burgher AH, Pope JE, Gilmore CA, Qureshi FA, Staats PS, Scowcroft J, Carlson J, Kim CK, Yang MI, Stauss T, Poree L; Evoke Study Group. Long-term safety and efficacy of closed-loop spinal cord stimulation to treat chronic back and leg pain (Evoke): a double-blind, randomised, controlled trial. Lancet Neurol. 2020 Feb;19(2):123-134. doi: 10.1016/S1474-4422(19)30414-4. Epub 2019 Dec 20.
This webinar has been supported by an educational grant from Saluda Medical.
The Development of a Novel Spinal Cord Stimulation Therapy
Thursday, Oct. 7, 2021
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert M. Levy, MD, PhD and Stana Bojanic, BSc (Hons), MB BS, FRCS (SN)
Faculty and Topics
Theory, Hypothesis and Animal Testing – James Makous, PhD
Clinical Trials to Test Efficacy: Acute Studies – Ganesan Baranidharan, MD, MBBS, FRCA, FFPMRCA, PG Dip (anaes)
Clinical Trials to Test Efficacy: Chronic Studies – Paul Verrills, MBBS, FAFMM, GDMM (Hons), MM (Pain Medicine), FIPP
Background
1. Staats P, Hartley L, Mishra LN, et al. Human Comfort and Feasibility Data from a New, Miniaturized SCS System. presented at: North American Neuromodulation Society (NANS) Meeting; January 17-January 20 2019; Las Vegas: https://doi.org/10.1111/ner.13133
2. Amirdelfan K, Levy R, Poree L, Staats P. Evaluation of a New, Battery-Free Microstimulator SCS System: Comfort and Ease-of-Use Data (nPower™ study). presented at: North American Neuromodulation Society (NANS) Meeting; January 23-January 26 2020; Las Vegas: https://doi.org/10.1111/ner.13133
3. Amirdelfan K, Levy R, Poree L, et al. Evaluation Of a New, Battery-Free Micro-Implantable Pulse Generator SCS System: Patient Choice, Comfort and Ease-of-Use Data. presented at: North American Neuromodulation Society (NANS) Meeting; January 23-January 26 2020; Las Vegas: https://doi.org/10.1111/ner.13133
This webinar was supported by an educational grant from Nalu Medical.
Differential Target Multiplexed Spinal Cord Stimulation
Thursday, Sept. 9, 2021
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert M. Levy, MD, PhD and Sarah Love-Jones, MBBS
Faculty and Topics
The Role of Glial Cells in Spinal Cord Stimulation – David Cedeño, PhD
The Basic Science Supporting Differential Target Multiplexed Therapy – Ricardo Vallejo, MD, PhD
The Clinical Evidence Supporting Differential Target Multiplexed Therapy – Michael Fishman, MD, MBA
Background
1) Cedeño DL, Smith WJ, Kelley CA, Vallejo R. Spinal cord stimulation using differential target multiplexed programming modulates neural cell-specific transcriptomes in an animal model of neuropathic pain. Molecular Pain. January 2020. doi:10.1177/1744806920964360
2) Vallejo R, Kelley CA, Gupta A, Smith WJ, Vallejo A, Cedeño DL. Modulation of neuroglial interactions using differential target multiplexed spinal cord stimulation in an animal model of neuropathic pain. Molecular Pain. January 2020. doi:10.1177/1744806920918057
3) Fishman, M.A., Calodney, A., Kim, P., Slezak, J., Benyamin, R., Rehman, A., Soto, E., Yang, T., Hacobian, A., Griffith, L., Yu, C. and Vallejo, R. (2020), Prospective, Multicenter Feasibility Study to Evaluate Differential Target Multiplexed Spinal Cord Stimulation Programming in Subjects With Chronic Intractable Back Pain With or Without Leg Pain. Pain Pract, 20: 761-768. https://doi.org/10.1111/papr.12908
This webinar has been supported by an educational grant from Medtronic.
Neuromodulation for Peripheral Neuropathic Pain
Tuesday, Aug. 24, 2021
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert M. Levy, MD, PhD and Marc A. Russo, MBBS DA (UK) FANZCA FFPMANZCA
Faculty and Topics
Basic Science / Animal Models of Neurostimulation for Peripheral Neuropathy Pain – Elbert Joosten, PhD
Meta-analysis of the Literature for Neurostimulation for Peripheral Neuropathy Pain – James FitzGerald, MA, BM, BCh, FRCS(SN), PhD
High Frequency Stimulation at 10 kHz for Peripheral Polyneuropathy – Erika A. Petersen, MD, FAANS, FACS
Dorsal Root Ganglion Stimulation for Peripheral Neuropathy Pain – Sam Eldabe, MB ChB FRCA
This webinar has been supported by an educational grant from Nevro.
Restorative Neurostimulation for Chronic Mechanical Back Pain
Thursday, July 1, 2021
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert M. Levy, MD, PhD and Erika A. Petersen, MD, FAANS, FACS
Faculty and Topics
The Use of Peripheral Nerve Stimulation to Improve Multifidus Muscle Function – Krishnan Chakravarthy, MD, PhD
The Anatomy and Physiology of Chronic Mechanical Back Pain – Marc A. Russo, MBBS DA (UK) FANZCA FFPMANZCA
The Clinical Data Supporting the Use of Multifidus Stimulation for Chronic Mechanical Back Pain – Robert M. Levy, MD, PhD
Background
1. Russo, M., Deckers, K., Eldabe, S., Kiesel, K., Gilligan, C., Vieceli, J. and Crosby, P. (2018), Muscle Control and Non-specific Chronic Low Back Pain. Neuromodulation: Technology at the Neural Interface, 21: 1-9. https://doi.org/10.1111/ner.12738
2. Gilligan, Christophera,*; Volschenk, Willemb; Russo, Marcb; Green, Matthewc; Gilmore, Christopherd; Mehta, Viveke; Deckers, Kristiaanf; De Smedt, Krisg; Latif, Usmanh; Georgius, Peteri; Gentile, Jonathanj; Mitchell, Brucek; Langhorst, Meredithl; Huygen, Frankm; Baranidharan, Ganesann; Patel, Vikaso; Mironer, Eugenep; Ross, Edgara; Carayannopoulos, Alexiosq; Hayek, Salimr; Gulve, Ashishs; Van Buyten, Jean-Pierret; Tohmeh, Antoineu; Fischgrund, Jeffreyv; Lad, Shivanandw; Ahadian, Farshadx; Deer, Timothyy; Klemme, Williamz; Rauck, Richardaa; Rathmell, Jamesa; Levy, Robertab; Heemels, Jan Pieterac; Eldabe, Sams for the ReActiv8-B investigators An implantable restorative-neurostimulator for refractory mechanical chronic low back pain, PAIN: March 09, 2021 - Volume Articles in Press - Issue - doi: 10.1097/j.pain.0000000000002258
https://journals.lww.com/pain/Abstract/9000/An_implantable_restorative_neurostimulator_for.98100.aspx
This webinar was supported by an educational grant from Mainstay Medical.
Radiation in Interventional Procedures: Risks, Education, and Mitigation Strategies
Thursday, June 3, 2021
Visit the Member's Webinar Page for the recorded video and CME information.
Faculty and Topics
Radiation Safety: Understanding the Risk and Current State of Physician Competency – David Provenzano, MD
Best Practices for Radiation Safety and Protection – Carlos Pino, MD
Recommendations and Guidelines for Improving Radiation Education – Christine Hunt, DO
Background Articles
Provenzano DA, Florentino SA, Kilgore JS, De Andres J, Sitzman BT, Brancolini S, Lamer TJ, Buvanendran A, Carrino JA, Deer TR, Narouze S. Radiation safety and knowledge: an international survey of 708 interventional pain physicians. Reg Anesth Pain Med. 2021 Mar 9:rapm-2020-102002. doi: 10.1136/rapm-2020-102002. Epub ahead of print. PMID: 33688038.
P. Ortiz Lopez, L.T. Dauer, R. Loose, C.J. Martin, D.L. Miller, E. Vaño, M. Doruff, R. Padovani, G. Massera, C. Yoder. ICRP, 2018. Occupational radiological protection in interventional procedures. ICRP Publication 139. Ann. ICRP 47(2).
Vagus Nerve Stimulation for Epilepsy
Polyanalgesic Consensus Conference (PACC)
Neuromodulation Appropriateness Consensus Committee (NACC)
Vagus Nerve Stimulation for Epilepsy Part 2
Contemporary Therapy
Thursday, May 6, 2021
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert M. Levy, MD, PhD and Jeffrey E. Arle, MD, PhD, FAANS
Topics
Patient Selection for Vagus Nerve Stimulation for Epilepsy – Arthur Cukiert, MD, PhD
Surgical Techniques for Vagus Nerve Stimulator Implantation – Jeffrey E. Arle, MD, PhD, FAANS
Vagus Nerve Stimulation Programming and Outcomes Assessment – Kristl Vonck, MD, PhD
This webinar has been supported by an educational grant from LivaNova USA, Inc.
Vagus Nerve Stimulation for Epilepsy Part 1
Basic and Clinical Science
Thursday, April 1, 2021
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert M. Levy, MD, PhD and Arthur Cukiert, MD, PhD
Faculty and Topics
Vagus Nerve Stimulation for Epilepsy - Basic Science and Mechanism(s) of Action – Kristl Vonck, MD, PhD
Predicting Success of Vagus Nerve Stimulation for Drug Resistant Epilepsy – George Ibrahim, MD, PhD, FRCSC
Vagus Nerve Stimulation for Epilepsy - Contemporary Clinical Outcomes – Paul Boon, MD, PhD
This webinar has been supported by an educational grant from LivaNova USA, Inc.

Webinar 4: Polyanalgesic Consensus Conference (PACC)
Status of Intrathecal Pharmacotherapy for Pain 2021: Your Questions Answered
Tuesday, Feb. 9, 2021
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert M. Levy, MD, PhD
Timothy R. Deer, MD
Faculty and Topics
General Questions About the PACC – Jay Grider, DO, PhD, MBA
Pharmacologic Considerations – Tony L. Yaksh, PhD
Trialing and Initiation of Intrathecal Therapy – Salim M. Hayek, MD, PhD
Clinical Care Guidance: Opioids – Magdalena Anitescu, MD, PhD
Clinical Care Guidance: Non-Opioids – Gladstone C. McDowell II, MD
Intrathecal Drug Delivery System Complications and Their Management – Lawrence R. Poree, MD, MPH, PhD
Webinar 3: Polyanalgesic Consensus Conference (PACC)
Intrathecal Drug Delivery - Algorithmic Approach to Intrathecal Drug Delivery for Different Pain Syndromes
Thursday, Jan. 7, 2021
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert M. Levy, MD, PhD
Timothy R. Deer, MD
Faculty and Topics
Patient Selection – Marc S. Wallace, MD
Trialing of Intrathecal Drug Delivery – Brian Bruel, MD
Intrathecal Drug Delivery for Cancer Pain – Denis Dupoiron, MD
Intrathecal Drug Delivery for Nociceptive Pain (FBSS) – Jason E. Pope, MD
Intrathecal Drug Delivery for Neuropathic Pain – Magdalena Anitescu, MD, PhD
ITDD for Complex Regional Pain Syndrome – Gladstone C. McDowell, II, MD
Webinar 2: Polyanalgesic Consensus Conference (PACC)
Intrathecal Drug Delivery - Complications and Management
Tuesday, Dec. 1, 2020
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert M. Levy, MD, PhD
Timothy R. Deer, MD
Faculty and Topics
Catheter Complications – Peter E. Konrad, MD, PhD
Catheter Tip Granulomas – Salim M. Hayek, MD, PhD
Pump Complications – Lawrence R. Poree, MD, PhD
Refill / Programming Complications – Padma Gulur, MD
Infection – David A. Provenzano, MD
Respiratory Depression and Drug Interactions – Philip S. Kim, MD
Webinar 1: Polyanalgesic Consensus Conference (PACC)
Status of Intrathecal Pharmacotherapy for Pain 2020
Thursday, Nov. 12, 2020
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert M. Levy, MD, PhD
Timothy R. Deer, MD
Faculty and Topics
Sam Eldabe, MB ChB FRCA – Intrathecal Opioids
Susan Moeschler, MD – Intrathecal Local Anesthetics
Christophe Perruchoud, MD – Intrathecal Alpha-2 Agonists
Jason E. Pope, MD – Intrathecal Ziconotide
Jay Grider, DO, PhD, MBA – Intrathecal Polypharmacy
Tony Yaksh, PhD – Novel Intrathecal Agents
References
- Deer TR, Pope JE, Hayek S, et al. The Polyanalgesic Consensus Conference (PACC): recommendations on intrathecal drug infusion systems best practices and guidelines. Neuromodulation . 2017;20(2):96-132. https://doi.org/10.1111/ner.12538
- Deer TR, Hayek S, Pope JE, et al. The Polyanalgesic Consensus Conference (PACC): recommendations for trialing of intrathecal drug delivery infusion therapy. Neuromodulation. 2017; 20(2):138-154. https://doi.org/10.1111/ner.12543
- Deer TR, Pope JE, Hayek S, et al. The Polyanalgesic Consensus Conference (PACC): recommendations for intrathecal drug delivery: guidance for improving safety and mitigating risk. Neuromodulation. 2017;20(2):155-176. https://doi.org/10.1111/ner.12579x
Webinar 6: Neurostimulation Appropriateness Consensus Committee (NACC)
Everything You Wanted to Know About Neuromodulation But Were Afraid to Ask
Thursday, Oct. 8, 2020
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert M. Levy, MD, PhD
Timothy R. Deer, MD
Faculty and Topics
Hematologic Issues in Neuromodulation – Marc Russo, MD
Infectious Disease Issues in Neuromodulation – Lawrence Poree, MD, PhD
Outcomes Assessment in Neuromodulation – Erika Petersen, MD
Questions Concerning Specific Technologies
Ricardo Vallejo, MD, PhD
Chris Gilligan, MD
Konstantin Slavin, MD
Corey Hunter, MD
Adnan Al-Kaisy, MD
Developing World Access to Neuromodulation – Fabian Piedimonte, MD, PhD
Webinar 5: Neurostimulation Appropriateness Consensus Committee (NACC)
Spinal Cord Stimulation: Regional Differences in Access and Policy
Thursday, Sept. 10, 2020
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators:
Robert M. Levy, MD, PhD
Timothy R. Deer, MD
Faculty and Topics:
Ganesan Baranidharan, MBBS – United Kingdom
Jan Vesper, MD, PhD – Germany
Richard Sullivan, MBCHB, FANZCA, FFPMANZCA – Australia
Kiran V. Patel, MD – USA
Fabián César Piedimonte, MD, PhD – South America
Tony Van Havenbergh, MD – Belgium
Webinar 4: Neurostimulation Appropriateness Consensus Committee (NACC)
Salvage for Failed Spinal Cord Stimulation Therapy: Case Presentations and Discussions
Wednesday, Aug. 19, 2020
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators:
Robert M. Levy, MD, PhD and Timothy R. Deer, MD
Faculty and Topics:
Corey W. Hunter, MD, FIPP – Dorsal Root Ganglion Stimulation Following SCS
Lawrence Poree, MD, MPH, PhD – Intrathecal Pump Following SCS
Erika A. Petersen, MD, FAANS, FACS – Burst Stimulation Following SCS
Thomas T. Simopoulos, MD, MA – High Frequency Spinal Cord Stimulation Following SCS
Simon Thomson, MBBS – 1kHZ and Less Subthreshold SCS Following SCS
Webinar 3: Neurostimulation Appropriateness Consensus Committee (NACC)
The Right Device for the Right Patient: Case Presentations and Discussions
Thursday, July 16, 2020
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators:
Robert M. Levy, MD, PhD and Timothy R. Deer, MD
Faculty and Topics:
Sam Eldabe, MBBS – Failed Back Surgery Syndrome
Adnan Al-Kaisy, MB ChB – Virgin Back
Corey Hunter, MD – Complex Regional Pain Syndrome
Konstantin Slavin, MD – Peripheral Nerve Pain
Julie Pilitsis, MD, PhD – Central Neuropathic Pain
Chris Gilligan, MD – Nociceptive Back Pain
Webinar 2: Neurostimulation Appropriateness Consensus Committee (NACC)
Novel Stimulation Technologies - Recent Research
Thursday, June 18, 2020
Visit the Member's Webinar Page for the recorded video and CME information.
Moderators
Robert Levy, MD, PhD
Stana Bojanic, BSc, MB BS, FRCS
Timothy R. Deer, MD
Faculty and Topics
Dirk De Ridder, MD, PhD – Burst Spinal Cord Stimulation
Adnan Al-Kaisy, MB ChB – The Role of 10 kHz SCS in the Management of Axial Lower Back Pain in Patients with No History of Spinal Surgery
Ricardo Vallejo, MD, PhD – Layered Stimulation Patterns
Marc A. Russo, MBBS DA (UK), FANZCA, FFPMANZCA – Feedback Loop in Spinal Cord Stimulation
Simon Thomson, MBBS, FRCA, FIPP, FFPMRCA – Sub-Perception SCS "Neural Dosing" Parameter Relationships
Christopher Gilligan, MD, MBA – Multifidus Muscle Stimulation for Refractory Chronic Low Back Pain
Webinar 1: Neurostimulation Appropriateness Consensus Committee (NACC)
Safety Guidelines for the Reduction of Severe Neurological Injury
Thursday, May 7, 2020
Visit the Member's Webinar Page for the recorded video and CME information.
Faculty and Topics
Robert Levy, MD, PhD, INS President – Welcome from the INS
Timothy Deer, MD, INS Immediate Past President – Overview of the Program and Discussion
Steven Falowski, MD – NACC Guidance on Neurological Injury with Neurostimulation
Leonardo Kapural, MD, PhD – NACC Guidance on Bleeding and Hemostasis during Neurostimulation
Adnan Alkaisy, MB ChB – NACC Guidance on Infection during Neurostimulation
Erika Peterson, MD – NACC Guidance on Grading and Ranking Evidence
Marc Russo, MBBS – NACC Key Points: What to Take Home to Your Practice
Questions from the Audience and Moderators – Panel Discussion
Timothy Deer, MD – Discussion of the Next NACC in 2021
Robert Levy, MD, PhD – Final Thoughts
Learning Objectives
As a result of participating in this webinar, attendees will be able to:
- Define the recommendations on improving safety and reducing the risks for neurostimulation techniques
- Describe the United States Preventive Services Task Force criteria for evidence synthesis and CDC evidence ranking
- Learn the appropriate measures to take to improve the safety of neurostimulation devices
Citations
The Neurostimulation Appropriateness Consensus Committee (NACC) Safety Guidelines
Deer, T. R., Lamer, T. J., Pope, J. E., Falowski, S. M., Provenzano, D. A., Slavin, K., Golovac, S., Arle, J., Rosenow, J. M., Williams, K., McRoberts, P., Narouze, S., Eldabe, S., Lad, S. P., De Andrés, J. A., Buchser, E., Rigoard, P., Levy, R. M., Simpson, B. and Mekhail, N. (2017), The Neurostimulation Appropriateness Consensus Committee (NACC) Safety Guidelines for the Reduction of Severe Neurological Injury. Neuromodulation: Technology at the Neural Interface. doi:10.1111/ner.12564
Deer, T. R., Provenzano, D. A., Hanes, M., Pope, J. E., Thomson, S. D., Russo, M. A., McJunkin, T., Saulino, M., Raso, L. J., Lad, S. P., Narouze, S., Falowski, S. M., Levy, R. M., Baranidharan, G., Golovac, S., Demesmin, D., Witt, W. O., Simpson, B., Krames, E. and Mekhail, N. (2017), The Neurostimulation Appropriateness Consensus Committee (NACC) Recommendations for Infection Prevention and Management. Neuromodulation: Technology at the Neural Interface. doi:10.1111/ner.12565
Deer, T. R., Narouze, S., Provenzano, D. A., Pope, J. E., Falowski, S. M., Russo, M. A., Benzon, H., Slavin, K., Pilitsis, J. G., Alo, K., Carlson, J. D., McRoberts, P., Lad, S. P., Arle, J., Levy, R. M., Simpson, B. and Mekhail, N. (2017), The Neurostimulation Appropriateness Consensus Committee (NACC): Recommendations on Bleeding and Coagulation Management in Neurostimulation Devices. Neuromodulation: Technology at the Neural Interface. doi:10.1111/ner.12542
CME Credit and Webinar Recording
This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through a collaboration between Elsevier, Inc. and the International Neuromodulation Society.
The Elsevier Office of CME is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
The Elsevier Office of CME designates this educational material for a maximum of 1.5 AMA PRA Category 1 Credit(s)™. Physicians should only claim credit commensurate with the extent of their participation in the activity. Each recorded presentation is eligible for CME credits for up to sixty (60) days after the date of a webinar event.
The webinars are recorded. Members may watch the videos on demand by logging on to the INS members' website.
If you are not currently an INS member and you would like to enjoy this and other society and regional chapter benefits, you are invited to join the INS or your local chapter at: https://www.neuromodulation.com/become-a-member .
CME Credit for Programs Prior to March 2022
This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of Evolve Medical Education, LLC and the International Neuromodulation Society (INS). Evolve Medical Education, LLC is accredited by the ACCME to provide continuing medical education for physicians.
Evolve Medical Education designates this live activity for a maximum of 1.50 AMA PRA Category 1 CreditsTM. Physicians should claim only the credit commensurate with the extent of their participation in the activity. Each recorded presentation is eligible for CME credits for up to one year after the date of a webinar event.
|